2010
HCC detection in pre-transplant patients: A comparative retrospective study between multiphasic CT, gadoxetic acid-enhanced MRI and extracellular gadolinium based contrast-enhanced MRI1Radiology, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 2Department of Pathology, Icahn School of Medicine at Mount Sinai, New York, NY, United States, 3Translational and Molecular Imaging Institute, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Synopsis
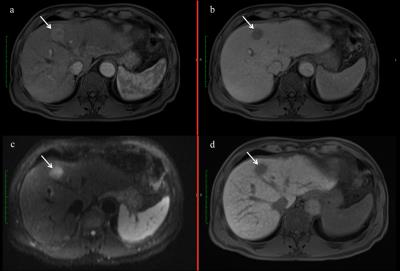
In this study, we present preliminary data comparing the diagnostic performance of multiphasic contrast-enhanced CT with contrast enhanced MRI using a liver specific gadolinium based contrast agent (GBCA), gadoxetic acid (Gd-EOB-DTPA) and extracellular (EC) GBCAs, using explant pathologic data as the reference. We also assessed the added value of delayed hepatobiliary phase (HBP) imaging and DWI in HCC detection. Our data suggests that CT and MRI have similar overall sensitivities for HCC detection and that the addition of DWI and HBP improved HCC detection when using Gd-EOB-DTPA.
Purpose
Hepatocellular carcinoma (HCC) is the most common primary hepatic malignancy, and is considered the second most common cause of cancer-related death worldwide [1]. The United Network for Organ Sharing allows allocation of patients for liver transplantation, a curative treatment for HCC, based on imaging findings on multiphasic contrast-enhanced CT or MRI [2]. With Gd-EOB-DTPA, delayed T1W-HBP (hepatobiliary phase) images can be obtained, which have been shown to improve HCC detection [3]. There is limited data comparing the performance of MRI using extracellular (EC) gadolinium based contrast agents (GBCAs) vs. Gd-EOB-DTPA. The goal of this study is to assess the diagnostic performance of multiphasic CT with MRI using EC GBCAs versus Gd-EOB-DTPA for HCC detection, and to assess the added use of DWI and HBP, using explant pathology as the reference.Materials and Methods
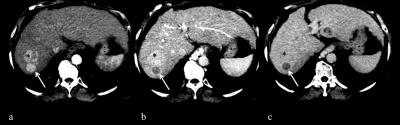
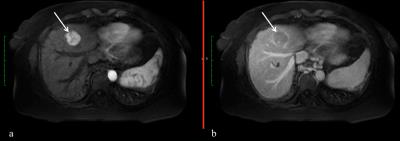
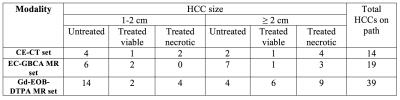
Initial data (n=59, 39M/20F, mean age 59y) from a single center retrospective IRB approved study involving 300 patients are presented. Patients who underwent cross-sectional imaging within 90 days of liver transplant, between January 2008 and October 2015, were included and divided into 3 groups: 1) multiphasic CT (n=20), 2) MRI with EC GBCA (n=19), and 3) MRI with Gd-EOB-DTPA, including only dynamic MRI (n=20). Two radiologists were asked to record all liver lesions measuring ³1cm and characterize them based on OPTN and LI-RADS criteria,. The observers were blinded to the radiology report and pathologic findings. Many patients had received locoregional therapy prior to imaging, and some lesions were necrotic. In these cases, the readers were asked to specify the percent necrosis of the lesions and indicate if there was a viable component. Group 3 was re-evaluated after two weeks with the addition of DWI and T1w-HBP. The results were correlated with explant pathologic findings by the study coordinator. Per-patient and per-lesion sensitivities were calculated, for lesions diagnosed as HCC on imaging as OPTN 5/LI-RADS 5 (Fig. 1-3). False positive rates were also measured for each group.Results
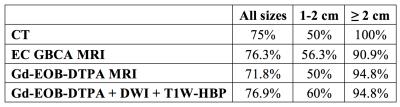
A total of 72 HCCs (2.4±1.4 cm) were diagnosed on pathology in 36/59 patients. Out of these tumors, 35 had been previously treated, with 22 being completely necrotic (Table 1). In group 1 (CT), per-patient sensitivities were equivalent for both observers at 90%. In group 2 (MRI with EC-GBCA), per-patient detection sensitivities were 89%-100% for observer 1 and 2, respectively. In group 3 (MRI with Gd-EOB-DTPA), per-patient detection sensitivities were 100%-100% without and with consideration of DWI and T1-HBP features. The per-lesion sensitivities were calculated for each group and further stratified based on size criteria (Table 2). Overall per-lesion sensitivities were similar among the 3 groups, regardless of lesion size. False Positive (FP) lesions: For observer 1, there was 1 FP lesion in the CT set, and none in the MRI sets. For observer 2, there was 1 FP lesion in the CT set, 1 in the EC-GBCA MRI set, and none in the Gd-EOB-DTPA MRI set.Discussion
Our preliminary results show similar overall per-patient sensitivities for HCC detection for multiphasic contrast-enhanced CT, MRI with EC-GBCA, and MRI with Gd-EOB-DTPA, ranging from 89%-100%. Per-lesion sensitivities were also relatively comparable for the 3 groups, both for HCCs measuring 1-2 cm and those measuring ≥2 cm, with improved detection sensitivity for the larger lesions. Our preliminary results contradict findings from previous studies that describe superior diagnostic performance of Gd-EOB-DTPA enhanced MRI compared to CT [4]. A possible explanation for this is the larger number of HCCs per-patient in the MRI groups, which may make interpretation of findings more challenging. Additionally, our data found that the HCC detection sensitivity of Gd-EOB-DTPA enhanced MRI is improved with the addition of DWI and T1W-HBP sequences, supporting findings from prior studies [5]. This is particularly evident for lesions smaller than 2 cm.Conclusion
Preliminary data from this retrospective study suggests comparable per-lesion and per-patient sensitivity for HCC detection using multiphasic CT and MRI using both EC-GBCA and Gd-EOB-DTPA. Our data also suggests improved performance of Gd-EOB-DTPA enhanced MRI with the addition DWI and T1W-HBP for HCCs smaller than 2 cm. Future plan is to analyze a larger number of cases.Acknowledgements
No acknowledgement found.References
1. Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87-108.
2. Wald C, Russo MW, Heimbach JK, Hussain HK, Pomfret EA, Bruix J. New OPTN/UNOS policy for liver transplant allocation: standardization of liver imaging, diagnosis, classification, and reporting of hepatocellular carcinoma. Radiology. 2013;266(2):376-382.
3. Lee DH, Lee JM, Baek JH, Shin CI, Han JK, Choi BI. Diagnostic performance of gadoxetic acid-enhanced liver MR imaging in the detection of HCCs and allocation of transplant recipients on the basis of the Milan criteria and UNOS guidelines: correlation with histopathologic findings. Radiology. 2015;274(1):149-160.
4. Guo J, Seo Y, Ren S, et al. Diagnostic performance of contrast-enhanced multidetector computed tomography and gadoxetic acid disodium-enhanced magnetic resonance imaging in detecting hepatocellular carcinoma: direct comparison and a meta-analysis. Abdom Radiol. 2016;41(10):1960-1972.
5. Park MS, Kim S, Patel J, et al. Hepatocellular carcinoma: detection with diffusion-weighted versus contrast-enhanced magnetic resonance imaging in pretransplant patients. Hepatology. 2012;56(1):140-148.
Figures