2005
The predictive value of diffusion-weighted imaging on radiation-induced liver injury of hepatic malignancies1Diagnostic Radiology, Cancer Hospital, Chinese Academy of Medical Sciences, Peking Union Medical College, Beijing, People's Republic of China
Synopsis
Radiation-induced liver injury (RILI) is one of the most dreaded complications of radiation therapy (RT),which prevents radiation dose escalation and limits the effectiveness of the treatment . Therefore, it was important to predict and evaluate the RILI on hepatic malignancy using the RT in the early term. In this study, the ADCmid-RT value was significantly highest, and had negative correlation with the radiation dose. As the ADCmid-RT value was less than 1.29 x10-3mm2/s, the RILI could possibly occur. Therefore, the ADCmid-RT value may serve as a biomarker for predicting RILI in patients with hepatic malignancies treated with RT.
Body
Introduction: Radiation-induced liver injury (RILI) is one of the most dreaded complications of radiation therapy (RT),which prevents radiation dose escalation and limits the effectiveness of the treatment [1]. No known method can effectively treat the RILI today [2]. Therefore, it became a very important research topic to predict and evaluate the RILI on hepatic malignancy before and after the RT in the early term by exploring the precise parameters and cutoff values of MRI. The purpose of this study was to explore the efficacy of DWI for predicting RILI at different time points of RT (pre-RT, mid-RT).
Materials and methods: 30 patients with hepatic malignancies included 16 hepatocellular carcinoma (HCC) of post-hepatectomy, 8 HCC of post- Transcatheter arterial chemoembolization (TACE), 3 cholangiocarcinoma and 3 recurrence after liver transplantation. All patients underwent DWI (b=0, 800 s/mm2) and conventional MRI on a 3.0T MR scanner at three time points: before start of RT(pre-RT), during treatment(mid-RT ,at the dose of 25Gy) and after the end of RT (conventional treatment completed, post-RT). Meanwhile, the patients were as follows: (1) availability of dose metric parameters of RT and (2) follow-up times ≥3 months, with available biochemical profiles after RT. The ADC values were measured on liver region with the matching dose metric map at pre-, mid- and post-RT. Regions of interest (ROI) were drawn by manually according to the different dose distribution in the liver parenchyma. All data were statistically analyzed.
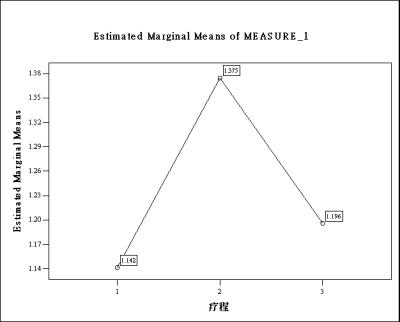
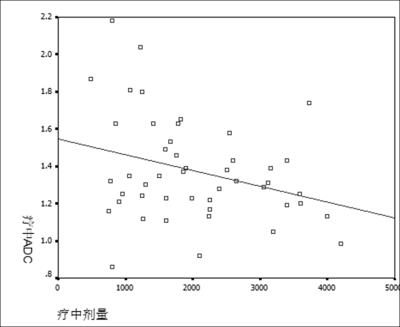
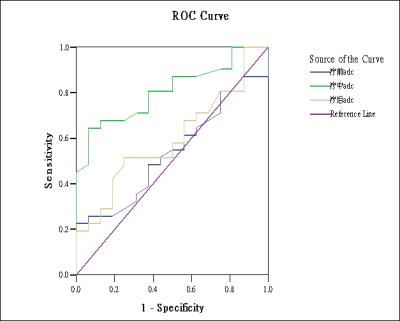
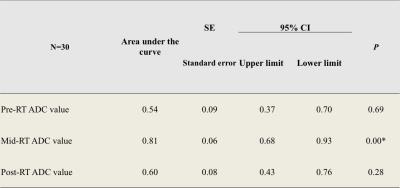
Results: The mean ADC values of liver parenchyma in the target region at pre-RT, mid-RT and post-RT were significantly different ((1.14±0.27) x10-3mm2/s, (1.37±0.28) x10-3mm2/s , (1.20±0.32) x10-3mm2/s; P<0.05, respectively). Especially, the mid-RT ADC value elevated significantly among the different period ADC values (Fig1). The negative correlation between mid-RT ADC value and radiation dose was seen for the irradiated livers (r= -0.36, P=0.03) (Fig2). When ROC of was used for finding the diagnostic ability and determining the cut-off value, the mid-RT ADC value was significantly correlated with the RILI of the irradiated livers (Fig3, Table1). The cut-off value of mid-RT ADC value was 1.29 x10-3mm2/s. As the mid-RT ADC value was less than 1.29 x10-3mm2/s, the RILI could possibly occur (sensitivity=64.5(95%CI,45.4-80.8%), specificity=93.8%(95%CI,69.8-99.8%)).
Discussion: In recent years, DWI technology has been widely used in diagnosis of liver diseases, and in the evaluation and prediction of HCC treatment [3]. However, the prediction and evaluation of hepatic malignancies using RT on the human has been reported rarely. In this study, The ADC values were significantly different among the three time points (pre-RT, mid-RT and post-RT). Meanwhile, the mid-RT mean ADC value was significantly highest, and had negative correlation with the radiation dose. DWI is sensitive to microscopic motion of water molecules in the extra-vascular extracellular space (EES) [4], that might be related to the changes of ADC values at the three time points. However, we found the cutoff value of mid-RT ADC. The sample size of this study was relatively small.
Conclusion: DWI has high sensitivity for detecting RILI at three time points (pre-RT, mid-RT and post-RT). Meanwhile, the mid-RT mean ADC value was significantly highest, and had negative correlation with the radiation dose. As the mid-RT ADC value was less than 1.29 x10-3mm2/s, the RILI could possibly occur. Therefore, the mid-RT mean ADC value may serve as a biomarker for predicting RILI in patients with hepatic malignancies treated with RT.
Acknowledgements
No acknowledgement found.References
[1] Benson R, Madan R, Kilambi R, et al. Radiation induced liver disease: A clinical update. J Egypt Natl Canc Inst. 2016; 28(1):7-11.
[2] Kalogeridi MA, Zygogianni A, Kyrgias G, et al. Role of radiotherapy in the management of hepatocellular carcinoma: A systematic review. World J Hepatol. 2015; 7(1): 101-112.
[3] Lewis S, Dyvorne H, Cui Y, et al. Diffusion-weighted imaging of the liver: techniques and applications. Magn Reson Imaging Clin N Am. 2014; 22(3): 373-395.
[4] Sahin H, Harman M, Cinar C, et al. Evaluation of treatment response of chemoembolization in hepatocellular carcinoma with diffusion-weighted imaging on 3.0-T MR imaging. J VascIntervRadiol.2012; 23(2): 241-247.
Figures