1996
MRI of Liver Cysts in Autosomal Dominant Polycystic Kidney Disease: Effect of Genotype1Radiology, Weill Cornell Medicine, New York, NY, United States, 2Nephrology, Weill Cornell Medicine, New York, NY, United States, 3Radiology, Columbia University, New York, NY, United States
Synopsis
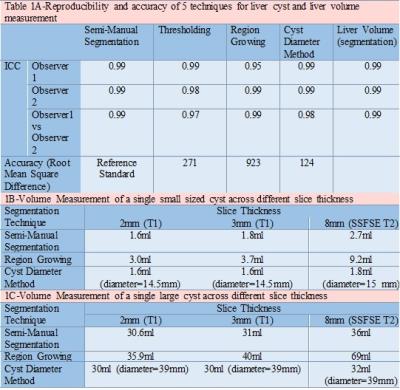
ADPKD patients (n=25) undergoing abdominal MRI were analyzed 2 times each by 2 separate reviewers using a) thresholding; b) region growing c) cyst diameter d) semi-manual segmentation to determine liver cyst volume. Using the most reproducible technique, 75 additional ADPKD patients were studied correlating their liver parameters with genotype, gender and age. Semi-manual segmentation was the best technique for measuring cyst volume with intraclass correlation coefficient of 0.99. PKD1 mutation was found to be associated with higher total liver volume and liver cyst volume across different age groups and gender compared to PKD2 mutation, suggesting greater hepatic involvement with PKD1.
Purpose
Cystic involvement of the liver is the most common extra-renal manifestation of autosomal dominant polycystic kidney disease (ADPKD) and in severe cases may result in massive hepatic enlargement causing considerable morbidity 1,2. ADPKD has been primarily associated with mutations in either PKD1 or PKD2 gene. The effect of PKD1 vs. PKD2 mutations on renal disease has been studied in detail, however very little data exists regarding the effect of genotype on liver involvement, primarily due to the difficulty in measuring liver cyst volume. Here, we evaluate 4 methods for liver cyst volume measurement for reproducibility and accuracy relative to a reference standard of semi-manual segmentation. The best method is then used to compare liver parameters with genotype, age and gender.Methods
Single shot fast spin echo (SSFSE) axial images covering the entire liver from 25 ADPKD patients presenting for abdominal MRI as part of the Rogosin ADPKD registry during 2015 were analyzed 2 times each by 2 separate reviewers using a) thresholding; b) region growing c) cyst diameter d) semi-manual segmentation to determine liver cyst volume. Total liver volumes were also measured 2 times each by the 2 reviewers. Inter-observer and intra-observer variability was assessed with intraclass correlation coefficients (ICC). Using the method of semi-manual segmentation, 75 additional ADPKD patients were studied. While evaluating liver parameters on MRI studies, both reviewers were blinded to genotypic and clinical characteristics of these patients. Multivariate linear regression analysis was performed to evaluate the effect of age, gender, and genotype on log transformed height adjusted liver volume.Results
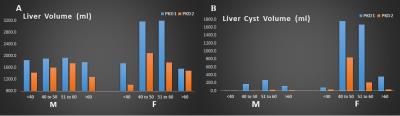
Semi-manual segmentation had the highest ICC (0.99) for both inter and intra-observer measurements, though other methods also had high reproducibility (ICC between 0.95-0.99). Liver volume measurements also had an ICC of 0.99 for both inter and intra-observer comparison (Figure 1). Liver and liver cyst volumes were found to be consistently higher among patients with PKD1 mutation when compared to patients with PKD2 mutation across different age groups and gender (Figure 2). On multiple regression analysis, PKD1 mutation is associated with higher liver volume (740ml on average) when compared to PKD2 mutation (p=0.03)Discussion
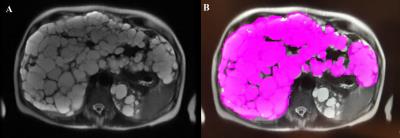
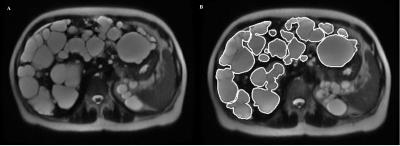
Semi-manual segmentation quantifies liver cyst volume with high reproducibility, but is the most time consuming technique averaging 7 minutes per case. Thresholding is limited by the presence of hyperintense hepatic vasculature on T2 images causing overestimation when there is a small number of cysts. However, in the presence of severe cystic disease thresholding performs well. Region growing is user friendly with good reproducibility. But its validity is questionable as it overestimates the burden of cystic disease due to its liberal extrapolation across the perpendicular, z, direction). Cyst diameter can be quickly measured, and this can be used to calculate cyst volumes using the formula for sphere volume. Volume of individual cysts calculated this way correlates well for small cysts. However, larger cysts that are not spherical due to their size or pressure effects from surrounding structures cannot be calculated accurately by this method. Furthermore, in a liver completely studded with cysts such as shown in Figure 3, identifying and measuring a diameter for each cyst becomes tedious and nearly impossible. In our cohort, two patients with hundreds of cysts could not be evaluated with this approach.
PKD1 mutation is associated with enlarged renal volumes at an earlier age, a higher number of renal cysts and earlier onset of end stage renal disease when compared to PKD2 mutation 3. The effect of ADPKD genotype on cystic involvement of liver has only been minimally studied, with no differences detected 4. Advancing age and female gender have long been regarded as worse prognostic factors for cystic involvement of liver in ADPKD patients 5, however no previous study has established a relationship between hepatic disease and ADPKD mutations. A small proportion of ADPKD patients go on to develop massive hepatic enlargement due to cystic involvement resulting in abdominal pain, early satiety, dyspnea, venous obstruction, portal hypertension, ascites as well as hemorrhagic cysts, infected cysts and rarely squamous cell carcinoma arising from cyst epithelium 1,2. All patients with massive hepatic enlargement (height adjusted liver volume >1800ml/m 5) in our study population were determined to have PKD1 mutation.
Conclusion
We have found semi-manual segmentation to be the best, albeit not the fastest technique for characterizing the volume of liver and cysts in patients with ADPKD. Using this method, we have found the PKD1 mutation to be associated with higher liver and liver cyst volumes when compared to PKD2 mutation.Acknowledgements
Study supported by National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (UL1RR024143)References
1.Van Keimpema L, De Koning DB, Van Hoek B et al. Patients with isolated polycystic liver disease referred to liver centres: clinical characterization of 137 cases. Liver Int. 2011 Jan;31(1):92-8.
2.Macutkiewicz C, Plastow R, Chrispijn M et al. Complications arising in simple and polycystic liver cysts. World J Hepatol. 2012 Dec 27;4(12):406-11.
3.Rossetti S, Harris PC. Genotype-phenotype correlations in autosomal dominant and autosomal recessive polycystic kidney disease. J Am Soc Nephrol. 2007 May;18(5):1374-80.
4.Chebib FT, Jung Y, Heyer CM, Irazabal MV et al. Effect of genotype on the severity and volume progression of polycystic liver disease in autosomal dominant polycystic kidney disease. Nephrol Dial Transplant. 2016 Jun;31(6):952-60.
5.Hogan MC, Abebe K, Torres VE, et al. Liver Involvement in Early Autosomal Dominant Polycystic Kidney Disease. Clinical gastroenterology and hepatology?: the official clinical practice journal of the American Gastroenterological Association. 2015;13(1):155-164.e6.
Figures