1875
White matter abnormalities of brain and cervical spinal cord in Hepatic Myelopathy patients: a diffusion tensor imaging study1Department of Radiology, Xijing Hospital, The Fourth Military Medical University, shaanxi, xi'an, People's Republic of China, 2School of Life Sciences and Technology, Xidian University, People's Republic of China, 3the fourth military medical university, People's Republic of China, 4School of Life Sciences and Technology, Xidian University, xi'an, People's Republic of China
Synopsis
The prominent syndrome of HM such as spastic paraparesis is usually considered resulting from abnormal function of thoracic segments, nevertheless, the involvement of intracranial fibers and cervical spinal cord is not clear. In this study, we found a widespread and robust white matter tract abnormality in brain of HM and non-HM patients, without significant difference with cervical spinal cord. Our finding may help shedding light on the underlying pathological mechanism of HM.
Abstract
Objective: Hepatic myelopathy (HM) is a rare clinical pathological syndrome occurring in 2%-4% of various chronic liver diseases with extensive portosystemic shunt, or results from intervention such as transjugular intrahepatic portosystemic shunt (TIPS). The prominent syndrome of HM such as spastic paraparesis is usually considered resulting from abnormal function of thoracic segments, nevertheless, the involvement of intracranial fibers and cervical spinal cord is not clear. This study is aiming at partly revealing the pathogenesis of HM, especially in intracranial fibers and cervical spinal cord.
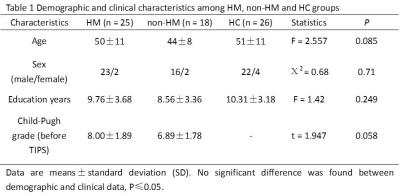
Methods: We used cross-sectional design to compare 25 HM patients after TIPS, 18 patients without HM after TIPS and 26 age-matched healthy controls. All subjects were scanned on a 3T scanner (Siemens Magnetom Trio Tim scanner, 3.0T). Voxel-wise Tract-based spatial statistics (TBSS) analysis of brain white matter fibers was performed using FMRIB Software Library (FSL, version 5.0.4; http://www.fmrib.ox.ac.uk). Cross-sectional area measurements and DTI parameters of cervical spinal cord were evaluated by SCT (spinal cord toolbox).
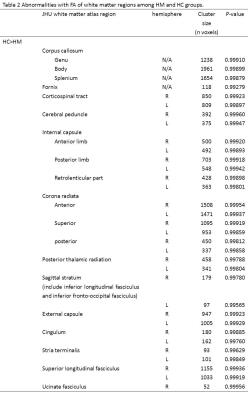
Results: In this study, we found a widespread and robust white matter tract abnormality in brain of HM and non-HM patients, involving association fibers, callosal fibers, thalamic fibers, limbic system fibers and projection fibers (especially corticospinal tract), without significant alterations of cervical spinal cord. In specific, by quantifying DTI metrics of white matter in brain using TBSS approach, we found extensive and unequivocal differences between patient groups (both HM and non-HM group) and healthy controls in FA, MD, AD and RD, as well significant differences between HM and non-HM groups. Furthermore, by objectively quantifying characteristic of spinal cord, we did not found any significant difference in aspect of cross-sectional area and DTI parameters at C1, C2, C3, C4 and C5 levels of cervical spinal cord.
Discusison: The prominent syndrome of HM such as spastic paraparesis is usually considered resulting from abnormal function of thoracic segments, nevertheless, the involvement of intracranial fibers and cervical spinal cord is not clear. Our finding may help shedding light on the underlying pathological mechanism of HM, namely the limited effect of cervical spinal cord aberration, thus possibly emphasizing the important role of intracranial corticospinal tract and thoracic spinal cord in the genesis and development of HM.
Acknowledgements
No acknowledgement found.References
1. Cohen-Adad J, El Mendili MM, Morizot-Koutlidis R, et al. Involvement of spinal sensory pathway in ALS and specificity of cord atrophy to lower motor neuron degeneration. Amyotroph Lateral Scler Frontotemporal Degener. 2013;14(1):30-8.
2. Utku U, Asil T, Balci K, Uzunca I, Celik Y. Hepatic myelopathy with spastic paraparesis. Clin Neurol Neurosurg. 2005;107(6):514-6.