1814
Can DTI Predict the MRI Level of Injury in Pediatric Spinal Cord Injury Subjects?1Radiology, Thomas Jefferson University, Philadelphia, PA, United States, 2Biostatistics Consulting Cente, Temple University School of Medicine, Philadelphia, PA, United States, 3Radiology, Temple University, Philadelphia, PA, United States, 4Occupational Therapy, Thomas Jefferson University, Philadelphia, PA, United States, 5Bioengineering, Temple University, Philadelphia, PA, United States
Synopsis
The purpose of this study was to determine whether DTI parameters can be used to predict the level of injury as observed on conventional MRI data in pediatric spinal cord injury (SCI) subjects and to estimate the cut points for the DTI parameters which best discriminates the abnormal MRI from normal appearing MRI regions. Ten subjects with chronic SCI underwent repeat axial DTI scans based on inner field of view sequence. FA, MD, AD and RD were calculated by using ROIs drawn on the whole cord along the entire spinal cord for both scans. FA, MD, RD were significant predictors of the MRI level of injury. The cut points for FA, MD, AD and RD discriminated the abnormal MRI from normal appearing MRI regions in these subjects. DTI has the potential to serve as a surrogate for an abnormal MRI level corresponding to a region of SCI in instances where the MRI scans are unavailable, unreliable or there is an equivocal clinical exam.
Purpose
The purpose of the study was two-fold: 1) To determine whether DTI parameters can be used to predict the level of injury as observed on conventional MRI data in pediatric spinal cord injury (SCI) subjects. 2) To estimate the cut points for the DTI parameters which best discriminates the abnormal MRI from normal appearing MRI regions.Methods
Subjects: Ten subjects with chronic SCI (mean age, 12.47±2.86) were recruited for this study. Written informed child assent and parental consent were obtained under the protocol approved by Institutional Review Board. Imaging: Subjects underwent repeat scans using 3.0T Verio MR scanner. The protocol consisted of conventional T1- and T2-weighted structural scans and axial DTI scans based on inner field of view sequence1. Axial diffusion tensor images were acquired by using 2 overlapping slabs in the same anatomic location prescribed for the T2-weighted images, to cover the cervical (C1-upper thoracic region) and thoracic (upper thoracic-L1) spinal cord. The imaging parameters included: 3 averages of 20 diffusion directions, 6 b0 acquisitions, b=800s/mm2, voxel size=0.8x0.8x6mm3, axial slices=40, TR=7900ms, TE=110ms, and TA=8:49min. Data postprocessing and analysis: After motion correction2 and tensor estimation3, DTI parameters; FA, MD, AD and RD were calculated by using ROIs drawn on the whole cord on grayscale FA maps at every axial slice (40 slices/scan) along the entire spinal cord for both scans. DTI parameters were quantified at each intervertebral disk level and at the mid-vertebral body level of the cervical and thoracic spinal cord in all subjects. Statistical analysis: Generalized estimating equations (GEE) were used to predict the level of injury by the DTI parameters. For each DTI parameter, the relationship of the parameter to injury was shown as the probability of MRI injury as a function of the parameter value. This method accommodates multiple measures per subject using an exchangeable correlation structure to model the multiple measurements per subject. The cut point analysis was also performed based on the sensitivity and specificity (Youden’s J) of the measurements. The cut point picked that point which was most discriminating between abnormal MRI and normal appearing MRI regions. All statistical analyses were performed with SAS, Version 9.4 (SAS Institute, Cary, North Carolina).Results
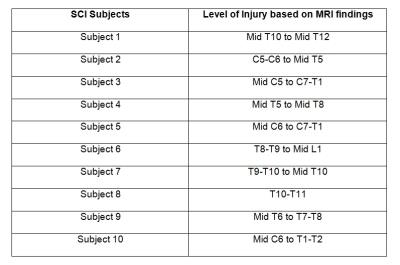
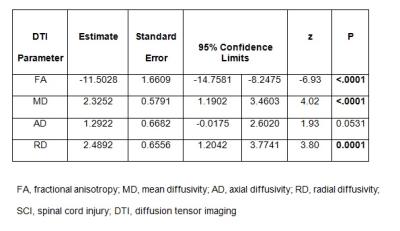
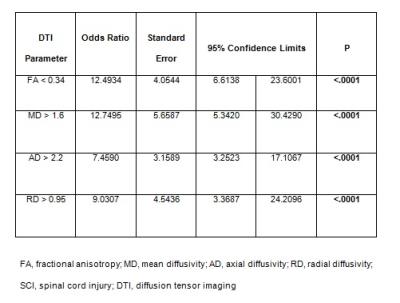
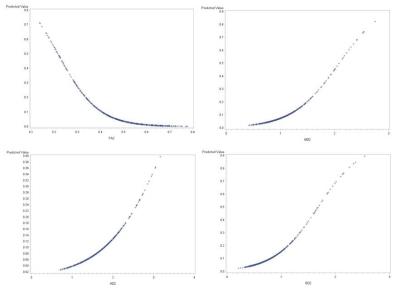
In all the 10 SCI subjects, the cord was abnormal at the level of injury on axial T2-weighted images. The level of injury based on conventional MRI findings is shown in Table 1. FA, MD, RD were significant predictors of the MRI level of injury (Table 2, Figure 1). The cut points for FA, MD, AD and RD discriminated the abnormal MRI from normal appearing MRI regions in these subjects (Table 3). The best cut point for FA was less than 0.34, for MD greater than 1.6, for AD greater than 2.20 and for RD greater than 0.95 (Table 3). It was also found that at these cut points the risk of injury increases 12.5 times if the FA value was less than 0.34, and 12.75 times if the MD value was greater than 1.6 mm2/sec, 7.5 times if the AD value is greater than 2.20 mm2/sec and 9.03 times if the RD value was greater than 0.95 mm2/sec (Table 3).Conclusion
Our results show that FA, MD and RD are significant predictors of MRI vertebral level of injury in SCI subjects. DTI has the potential to serve as a surrogate for an abnormal MRI level corresponding to a region of SCI in instances where the MRI scans are unavailable, unreliable or there is an equivocal clinical exam.Acknowledgements
This work was supported by National Institute of Neurological Disorders of the National Institutes of Health under award number R01NS079635.References
1. Finsterbusch J. Improving the performance of diffusion-weighted inner field-of-view echo-planar imaging based on 2D-selective radiofrequency excitations by tilting the excitation plane. J Magn Reson Imaging 2012;35:984–92.
2. Middleton DM, Mohamed FB, Barakat N, et al. An investigation of motion correction algorithms for pediatric spinal cord DTI in healthy subjects and patients with spinal cord injury. Magn Reson Imaging 2014;32:433-39.
3. Chang LC, Jones DK, Pierpaoli C. RESTORE: robust estimation of tensors by outlier rejection. Magn Reson Med 2005;53:1088-95.
Figures