1789
Characterization of the ulnar nerve using multislice DTI using a multiband factor of 1, 2, and 3Tina Jeon1, Ek Tsoon Tan2, Maggie Mei Kei Fung3, and Darryl B Sneag1
1Radiology and Imaging, Hospital for Special Surgery, New York, NY, United States, 2GE Global Research, Niskayuna, NY, United States, 3Apps & Workflow, GE Healthcare, New York, NY, United States
Synopsis
Multiband (MB) echo planar MR imaging (EPI) excites and refocuses multiple slice locations simultaneously using MB radiofrequency excitation and refocusing pulses that are subsequently un-aliased by exploiting differences in coil sensitivities. In this study, we investigated the feasibility of using MB diffusion tensor (DT) EPI with a multiband factor of 1, 2, and 3 to interrogate the ulnar nerve at different locations in the arm.
Purpose
In this study we investigated the feasibility of using simultaneously excited multi-slice echo planar imaging (EPI) acquired with diffusion magnetic resonance imaging (dMRI) to delineate the ulnar nerve. Multiband (MB) EPI can excite and refocus multiple slice locations simultaneously using multiband radiofrequency excitation and refocusing pulses which can be un-aliased by exploiting the differences in coil sensitivities. We hypothesize that MB DTI provides excellent SNR with the added incentive of faster scan time compared to conventional DTI. Here we aim to focus on interrogating the ulnar nerve at the level of the wrist, forearm and elbow with varying degrees of acceleration, MB factor=1, 2, and 3 and comparison of the DTI metrics.Methods
Subjects and data acquisition: 25 consented healthy volunteers (Figure 1) were scanned at the level of the elbow, wrist, and forearm on a GE 3T 60cm bore MR scanner (MR 750, GE Healthcare, Waukesha, WI, USA) using a 16 channel flexible extremity array in the superman position with echo planar MB and conventional DTI. The DWI parameters for the MB=2 and 3 are as follows: FOV:12cmx12cm, Matrix:128x128, TR/TE:2000/57.2ms, BW:195kHz, slice thickness:3mm, b=0,600s/mm2, 16 gradient directions, 4 NEX, MB factor=2, for a total scan time of 2:23 mins. Parameters for conventional DTI sequence (MB=1): FOV:12cmx12cm, Matrix:80x40, TR/TE:3500/66.1ms, BW:167kHz, slice thickness:3mm, b=0,600s/mm2, 16 directions, 4 NEX, with an adiabatic fat saturation pulse, for a total scan time of 3:48 mins. In-plane parallel imaging (ASSET=2) was used while none was applied to the MB acquisition. Tensor fitting and segmentation: The tensor fitting was conducted with the DWI of b=600s/mm2 to obtain the DTI maps using DTI Studio (mristudio.org). The ulnar nerve was extracted based on the contrast of the b=0 (Fig. 2). The fractional anisotropy (FA), mean diffusivity (MD), axial diffusivity (AD), and radial diffusivity (RD) were measured using the ulnar nerve as a mask. Paired t-test was used to test significant differences between regional DTI measures in the arm (alpha<0.05) and between the different MB acceleration factors.Results:
As shown in Fig. 2, the MB DTI (bottom two rows) shows improved SNR and delineation of anatomic structures compared to conventional DTI. For ulnar nerve MB DTI, the mean FA (0.52±0.04), AD (2.8x10-3mm±0.22), RD (1.27x10-3mm±0.2), and MD (1.67x10-3mm2/s±0.31) were similar to conventional DTI mean FA (0.47±0.08), AD (2.21x10-3mm±0.18), RD (1.0 x10-3mm±0.0), and MD (1.4x10-3mm2/s±0.12). There was no significant difference between MB DTI and conventional DTI for all measurements using paired t-test (p=0.42). As shown in Fig. 4, there is no difference in DTI metrics for all slices locations in the arm to interrogate the ulnar nerve.Discussion and conclusion:
Compared to conventional DTI, MB DTI provides excellent SNR with the added benefit of faster scan time, thus, can be optimized for higher in-plane spatial resolution. Many researchers have applied the MB DTI technique in the brain but to our knowledge, it has been rarely applied to peripheral nerves1-4. In the future, we hope to implement MB DTI clinically to interrogate the ulnar and other peripheral nerves as a possible mechanism to elucidate microstructure.Acknowledgements
This study is sponsored by GE Healthcare.References
[1] Larkman DJ et al, JMRI 13:313-317, 2001. [2] Setsompop K et al, MRM 67: 1210-1224, 2012. [3] Blaimer M et al, JMRI 24: 444-450, 2006. [4] Beatty PJ et al, ISMRM 2007 #1749.Figures
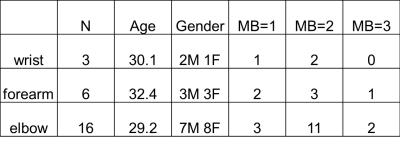
Figure 1: Subjects and demographics.
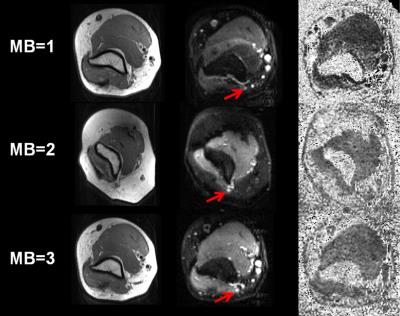
Figure 2: The axial proton density (left), b=0
(middle), and FA map (right) for multiband factors of 1, 2, and 3 in a normal
healthy volunteer at the level of the elbow. The red arrow is pointing to the
ulnar nerve in the non-diffusion weighted image, which was used to locate the
nerve.
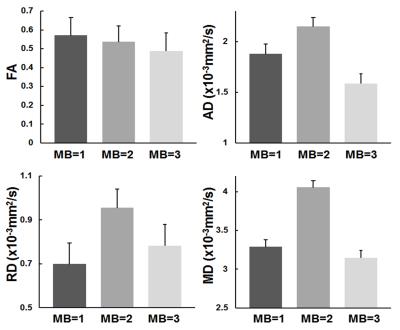
Figure 3: The mean of
the DTI metrics for different multi band acceleration factors.
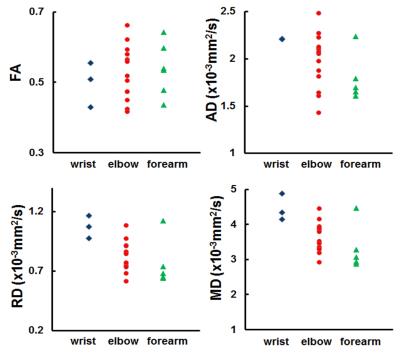
Figure 4:The DTI metrics in the at different slice locations in the arm.