1711
Altered Variability in Functional Connectivity of the Anterior Cingulate Cortex in Patients with Refractory and Nonrefractory Major Depressive Disorders1Radiology Department, West China Second University Hospital of Sichuan University, Chengdu, People's Republic of China, 2Huaxi MR Research Center, HMRRC, West China Hospital, Sichuan University, Chengdu, People's Republic of China, 3State Key Laboratory of Cognitive Neuroscience and Learning, Beijing Normal University, Beijing, People's Republic of China
Synopsis
Although substantial efforts have been made to elucidate the neuronal basis of both refractory MDD (rMDD) and nonrefractory MDD (nrMDD), the results are inconsistant. We apply the resting-state dynamic functional connectivity (D-RSFC) to explore the divergence of neuroal basis between rMDD and nrMDD. Our results demonstrated that the D-RSFC method can well reveal the dysfunctional brain networks in the MDD. The prefrontal-limbic circuit is the most stable dysfunctional brain network in both MDD subtypes. Additionally, we speculate that the OFC-sgACC circuit, especially the frontal part of the left OFC-sgACC circuit, might be the biomarker for evaluating treatment response in MDD.
Purpose
Major depressive disorder (MDD) is the most common unipolar affective disorder and is characterized by persistent and pervasive feelings of sadness, guilt, and worthlessness. Despite advances in the development of treatment strategies for MDD, up to 60% of MDD patients suffer at least one recurrence, and approximately 30% of patients do not respond to standard antidepressant treatment1. These patients are classified as having refractory MDD (rMDD), which adversely affects an individual’s normal life and general health and can lead to increased social and economic burdens2. Previous fMRI studies have related MDD to widespread local abnormalities in brain regions3. Although substantial efforts have been made to elucidate the neuronal basis of both refractory MDD (rMDD) and nonrefractory MDD (nrMDD), the results are inconsistant and little is known about whether or not there exist the divergent neuronal circuits between rMDD and nrMDD. We aim to assess the between-group differences of the mean strength and variance of the dynamical functional connectivity to explore the divergence of neuroal basis between rMDD and nrMDD.Methods
30 rMDD patients, 30 nonrefractory MDD patients and 30 healthy controls (HCs) underwent a resting-state fMRI scan with a 3-T MR system. The anterior cingulate cortex (ACC) was selected as the seed region. A variable parameter regression model combined with the Kalman filtering method4 was employed to detect the dynamic FC in the resting-state (D-RSFC) between the seed region and other voxels of the brain.Results
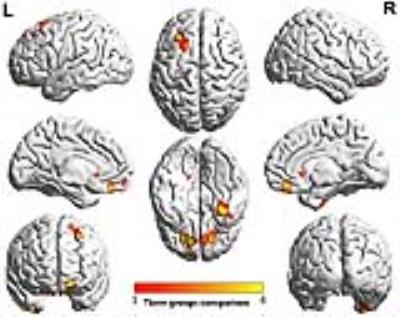
Widespread ACC D-RSFC patterns were found within each group (Figure 1). Among the three groups, significantly different D-RSFC were found in some frequently mentioned brain regions including bilateral orbitofrontal cortex (OFC), parahippocampus gyrus (PHG), prefrontal cortex and caudate (Figure 2). Relative to the HCs group, both MDD subtypes exhibited abnormal D-RSFC regions within cortical-limbic neural circuit (Figure 3). The rMDD exhibited higher D-RSFC values in left caudate relative to the nrMDD group (Figure 4). Nonetheless, nrMDD group showed more diverse abnormal D-RSFC regions than the rMDD group (Figure 3). Moreover, the D-RSFC between the ACC and the bilateral OFC showed significant correlation with the HAM-D score in the rMDD group.Discussion and Conclusion
Our results demonstrated that the prefrontal-limbic circuit is the most stable dysfunctional brain network in both MDD subtypes. The D-RSFC method can well reveal the altered dynamic functional connectivity in both MDD subtypes and the divergence of brain networks between rMDD and nrMDD. Additionally, we speculate that the caudate-ACC circuit might be the biomarker for evaluating treatment response in MDD. rmal D-RSFC regions within cortical-limbic neural circuit (Figure 3). The rMDD exhibited higher D-RSFC values in left caudate relative to the nrMDD group (Figure 4). Nonetheless, nrMDD group showed more diverse abnormal D-RSFC regions than the rMDD group (Figure 3). Moreover, the D-RSFC between the ACC and the bilateral OFC showed significant correlation with the HAM-D score in the rMDD group.Acknowledgements
This study was supported by the National Key Basic Research Program of China (973 Project, No. 2014CB846102), the National Natural Science Foundation (Nos. 81030027, 81030028, 811225012, 81227002, 31221003, and 81220108013, 81401479 and 91432115), the National Key Technologies R&D Program of China (No. 2012BAI01B03), the National Science Fund for Distinguished Young Scholars (No. 81225012), the Innovative Research Team in University (PCSIRT, No. IRT1272) of China, Chinese Postdoctoral Science Foundation (No. 2013M530401) and Beijing Funding for Training Talents (No. 2012D009012000003) and Beijing Natural Science Foundation (No. Z151100003915082).References
1.Smith, G.S., Kramer, E., Hermann, C., Ma, Y., Dhawan, V., Chaly, T., Eidelberg, D. (2009) Serotonin modulation of cerebral glucose metabolism in depressed older adults. Biol Psychiatry, 66:259-266.
2.Stimpson, N., AGRAWAL, N., LEWIS, G. (2002) Randomised controlled trials investigating pharmacological and psychological interventions for treatment-refractory depression Systematic review. Br J Psychiatry, 181:284-294.
3. Diener C, Kuehner C, Brusniak W, et al. A meta-analysis of neurofunctional imaging studies of emotion and cognition in major depression. Neuroimage 2012;61(3):677-685.
4. Kalman RE. A new approach to linear filtering and prediction problems. Journal of basic Engineering 1960;82(1):35-45.