1698
Resting State Brain Networks in Perinatally HIV-infected Adult Youths1Radiological Sciences, UCLA School of Medicine, Los Angeles, CA, United States, 2Biomedical Engineering, New Jersey Institute of Technology, Newark, NJ, United States, 3Pediatrics, Harbor-UCLA Medical Center, Torrance, CA, United States, 4Semel Institute for Neuroscience and Human Behavior, UCLA School of Medicine, Los Angeles, CA, United States, 5Radiology, Harbor-UCLA Medical Center, Torrance, CA, United States, 6Infectious disease-Pediatrics, Miller Children's Hospital, Long Beach, CA, United States, 7Pediatrics, UCLA School of Medicine, Los Angeles, CA, United States, 8Pediatrics, Keck School of Medicine of USC, Los Angeles, CA, United States, 9Psychiatry and Biobehavioral Sciences, UCLA School of Medicine, Los Angeles, CA, United States
Synopsis
Youths with perinatally infected HIV survive longer with combination antiretroviral therapy, but remain at risk for poor cognitive outcomes. Since changes in cognitive function may be preceded by subtle changes in brain function, resting-state functional magnetic resonance imaging (rs-fMRI) may become useful in evaluating functional connectivity in these youths. We evaluated alterations in brain functional connectivity in eight perinatally HIV-infected youths and eleven healthy controls. Results from this study demonstrate that, compared to normal subjects, the strength of the several networks connectivity including DMN, Dorsal Attention, Lateral Visual, were significantly decreased in several regions among perinatally HIV-infected youth. The detailed mechanisms, implications of these brain activities and networks exhibiting changes will require further investigation.
Introduction:
Although the tremendous success of combination antiretroviral therapy (ART) has transformed perinatal HIV into a chronic disease1-4, impairments in cognitive functioning are still being reported in HIV-infected patients5,6. Many children that have survived to adulthood from earlier eras with less efficacious regimens and may experience indolent ongoing brain injury. Since changes in cognitive function may be preceded by subtle changes in brain function, neuroimaging techniques, such as resting-state functional magnetic resonance imaging (rs-fMRI)7 can become useful tools in evaluating functional connectivity and assessing HIV-associated abnormalities in the brain. Although rs-fMRI has been used in many pathologies, however there are limited studies on brain connectivity alteration in HIV+ patients8-11, and only a few in perinatally HIV-infected children12. The purpose of the current study was to examine the extent to which HIV infection in perinatally HIV-infected Youth with ART is associated with disruptions in subcortical regions of the brain in comparison to a matched healthy control group. We hypothesize that that alterations in functional connectivity can be detected by rs-fMRI early in HIV infection.Materials and Methods:
We investigated eight perinatally HIV-infected youths (age 21.5 ± 2.1 years) and eleven healthy controls (HC) (age 22.18± 3.4). All subjects gave informed consent according to an institutionally approved research protocol. During the data acquisition, subjects were instructed to remain in a relaxed state with their eyes open and not to engage in any cognitive or motor activity. All data were collected on a Siemens 3T Prisma MRI scanner using a 16 channel head receive coil. rs-fMRI scans were collected using an echo planar imaging (EPI) sequence with: TR/TE=2000/27ms, Flip angle=900, 40 slices, matrix= 64x64; FOV=240 mm2; acquisition voxel size=3.75x3.75x4 mm3; and 180 volumes/scan. To facilitate EPI distortion correction, a field map was acquired before the rs-fMRI scan with: TR=430ms, TE=7.35/9.81ms, matrix=64x64, FOV=192mm, 40 4mm slices, no gap. In addition, a high-resolution T1-weighted magnetization-prepared rapid gradient echo scan (MPRAGE) was acquired for anatomical information for better registration and overlay of brain activity. Using pre-processing tools from Statistical Parametric Mapping (SPM8)13 and FSL14, raw EPI images were realigned, co-registered, normalized, and smoothed. Each of the data sets were pre-processed in an identical fashion: motion correction; spatial smoothing with 6 mm FWHM blur; temporal filtering in the LFF range of 0.01 to 0.10 Hz; removal of linear trends up to second order polynomials; and mapping of parameter values to 3mm MNI space. The resulting time-series data was then independently analyzed with Spatial independent component analysis (ICA) using Melodic software15. for each of the groups and 20 components was extracted from each of the groups.Results:
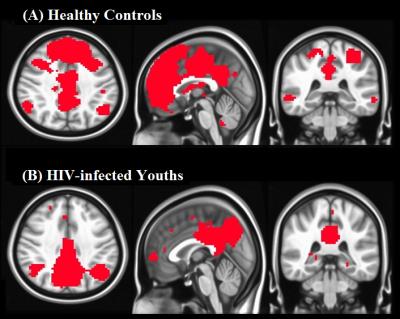
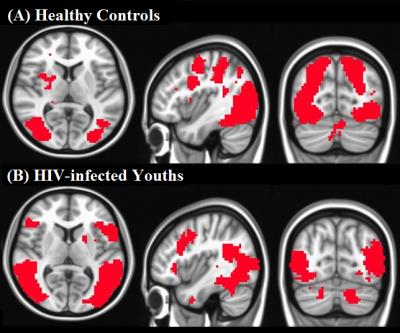
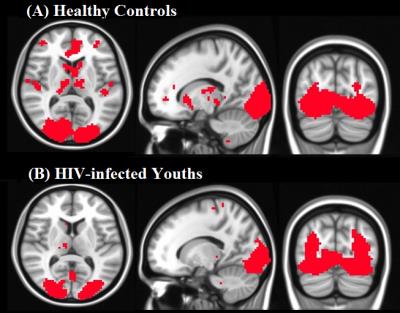
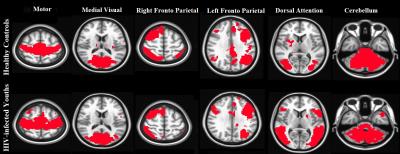
In Fig. 1(A) and 1(B) show the spatial extent of the default mode network (DMN) for the healthy subjects and HIV-infected youths, respectively. Among HIV-infected youths, a significant reduction in the activity can be observed in several regions. Fig. 2(A), 2(B) and 3(A), (B) show the dorsal attention and lateral visual networks respectively for the two groups. Significant reduction in activity can be observed in both the networks in HIV-infected youth compared to healthy controls. Fig. 4 shows the results for other 6 networks. Some reduction of activity was observed in dorsal attention and right fronto-parietal networks, but other networks do not show any changes.Discussion:
Results from this study demonstrate that, compared to normal subjects, the strength of the several networks connectivity including DMN, Dorsal Attention, and Lateral Visual were significantly decreased in several regions among perinatally HIV-infected youth. Our results of DMN activity reduction are in agreement with previous study12. Alterations in network DMN connectivity in HIV-infected youths may reflect global reorganization of the DMN which may ultimately relate to known cognitive processing difficulties in these youths. Weak Dorsal Attention, Lateral Visual and Dorsal Attention network connectivity in HIV-infected youth reflect the cognitive deficit observed in attention, speed of processing and visuospatial memory. Further studies with correlating these changes with neuropsychological test results and clinical parameters such as CD4 count, viral loads are required to confirm these changes. One of the limitations of the study is the small number of subject used. We intend to overcome these limitations using larger subject recruitment in the future.Conclusion:
Results from this study suggest that the resting state fMRI is a feasible tool for the evaluation of perinatally HIV-infected youth on ART. The detailed mechanisms, implications of these brain activities and networks exhibiting changes will require further investigation.Acknowledgements
This research was supported by NINDS 1R21-NS090956.References
1. Lee GM, Gortmaker SL, McIntosh K. Quality of life for children and adolescents: impact of HIV infection and antiretroviral treatment. Pediatrics. 2006;117:273-283.
2. Palella FJ Jr, Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338:853-860.
3. Tardieu M, Mayaux MJ, Seibel N, et al. Cognitive assessment of school-age children infected with maternally transmitted human immunodeficiency virus type 1. J Pediatr. 1995;126:375–379.
4. Patel K, Ming X, Williams PL, et al. International Maternal Pediatric Adolescent AIDS Clinical Trials 219/219C Study Team Impact of HAART and CNS-penetrating antiretroviral regimens on HIV encephalopathy among perinatally infected children and adolescents. AIDS. 2009;23:1893–1901.
5. Nagarajan R, Sarma MK, Thomas MA, et al. Neuropsychological function and cerebral metabolites in HIV-infected youth. J. Neuroimmune Pharmacol. 2012;7:981-990.
6. Smith R, Chernoff M, Williams PL, et al. Impact of HIV severity on cognitive and adaptive functioning during childhood and adolescence. Pediatr Infect Dis J. 2012;31:592–598.
7. Biswal B, Yetkin FZ, Haughton VM, Hyde JS. Functional connectivity in the motor cortex of resting human brain using echo-planar MRI. Magn Reson Med. 1995;34:537-541.
8. Wang X, Foryt P, Ochs R, et al. Abnormalities in resting-state functional connectivity in early human immunodeficiency virus infection. Brain Connect 2011; 1:207-217.
9. Thomas JB, Brier MR, Snyder AZ, et al. Pathways to neurodegeneration: effects of HIV and aging on resting-state functional connectivity. Neurology. 2013;80(13):1186-93.
10. Ann HW, Jun S, Shin NY, et al. Characteristics of Resting-State Functional Connectivity in HIV-Associated Neurocognitive Disorder. PLoS One. 2016;11(4):e0153493.
11. Janssen MA, Hinne M, Janssen RJ, et al. Resting-state subcortical functional connectivity in HIV-infected patients on long-term cART. rain Imaging Behav. 2016 [Epub ahead of print].
12. Herting MM, Uban KA, Williams PL, et al. Default Mode Connectivity in Youth With Perinatally Acquired HIV. Medicine (Baltimore). 2015;94(37):e1417.
13. Friston KJ. Statistical Parametric Mapping: the Analysis of Functional Brain Images. Elsevier/Academic Press, 2007.
14. Jenkinson M, Beckmann CF, Behrens TEJ, Woolrich MW, Smith SM. FSL. Neuroimage 2012; 62:782–790.
15. Beckmann CF, Smith SM. Probabilistic independent component analysis for functional magnetic resonance imaging. IEEE Trans Med Imaging. 2004; 23:137–152.
Figures