1636
Altered Spontaneous Brain Activity in Children with type 1 Gaucher disease: a Resting-state fMRI Study1Beijing children's hospital, Beijing, People's Republic of China, 2Research Center for Brain-inspired Intelligence, Institute of Automation, Chinese Academy of Sciences, Beijing, People's Republic of China
Synopsis
This is the first study to examine differences in spontaneous neural activity between GD patients and healthy controls. Our results indicate that decreased of neural activity in motor area; increased neural activity in the olfaction-, vision- and algesthesia -related structures; dysfunction of neural activity in emotion- , recognition- and speech- related structures and cerebellum. These results promote a further understanding of underlying neurophysiological mechanisms in the intrinsic brain of GD type I, which will aid in the development of treatment plans for GD type I patients that address both physical and psychological concern and preventing neurological disease in early stage.
PURPOSE
Gaucher disease(GD) is an autosomal recessive glycosphingolipid storage disorder. Main clinical manifestations include hepatosplenomegaly, pancytopenia, painful bone crises, osteonecrosis and osteopenia. According to clinical classification, three main phenotypes are distinguished.1-3 However, many patients do not fit into these categories. Recently, an epidemiological survey in GD type I patients found that a significant portion had neurological abnormalities.4,5 This study investigated the alterations of spontaneous brain activities in children with GD type I by resting-state functional magnetic resonance imaging (rs-fMRI).METHODS
We obtained rs-fMRI scans from 20 GD Type I children and 20 demographically matched healthy children. The amplitude of low-frequency fluctuation (ALFF), fractional ALFF (fALFF) and regional homogeneity (ReHo) of rs-fMRI data were calculated to measure spontaneous brain activity. Fisher’s r-to-z transformation was used to improve the normality of ALFF/fALFF and ReHo. A two-sample t test was performed to obtain functional differences between GD patients and normal controls (cluster-wised FDR corrected, p<0.01). Sperman correlation was performedto study the relationship between the GD abnormality and the clinical parameters (GD duration, age of onset, length of treatment and NGSS). The correlation was significant if the p-value is below 0.05.RESULTS
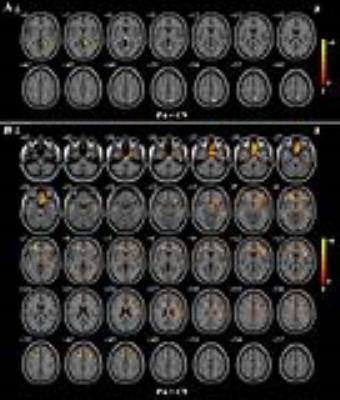
ReHo values were significantly increased in the right inferior frontal gyrus(pars opercularis), the right olfactory cortex, the left supplementary motor area and the left midcingulate area of GD patients while decreased values in the right precentral gyrus and the right postcentral gyrus of GD patients was observed. Increased ALFF were found in the right inferior frontal gyrus (pars opercularis), the right inferior frontal gyrus (pars triangularis), the right insula, the right inferior temporal gyrus, the right middle temporal gyrus, the left supplementary motor area and the right Rolandic operculum of GD patients when compared to the normal controls. Decreased ALFF were found in the right lingual gyrus, the left thalamus, the right precuneus and the right superior parietal lobule of GD patients. In GD patients, increased fALFF was also found in the left/right gyrus rectus, the left supplementary motor area, the right inferior frontal gyrus (pars opercularis), the left middle/ inferior occipital gyrus, the right inferior frontal gyrus (pars triangularis), the right insula, the right inferior temporal gyrus, the right precentral gyrus, the right lobule VI of cerebellar hemisphere, the left/ right lobule VIII of cerebellar hemisphere, the right crus I of cerebellar hemisphere and the left crus II of cerebellar hemisphere. Decreased fALFF was found in the right inferior parietal lobule, the right/left precuneus, the right midcingulate area and the left superior parietal lobule.After calculating the correlation coefficient between the abnormal functional indices of GD patients and clinical parameters, significantly negative correlation (r=-0.45, p=0.046) was observed between the ALFF of right precuneus and NGSS in GD patients. At the same time, significantly positive correlation (r=0.56, p=0.011) was observed between the ALFF of right precuneus and age of onset.DISCUSSION
Our results indicated that decreased of neural activity in motor area; increased neural activity in the olfaction-, vision- and algesthesia -related structures; dysfunction of neural activity in emotion- , recognition- and speech- related structures and cerebellum. Significantly negative correlation between the ALFF of right precuneus and NGSS represented the impairment of cognition consisting with the NGSS. Significantly positive correlation between the ALFF of right precuneus and age of onset represented the risk of cognition impairment increasing with age. These results promote a further understanding of underlying neurophysiological mechanisms in the intrinsic brain of GD type I and an increased knowledge about the emotional health of GD type I children.CONCLUSION
Our study is the first to evaluate the relationship between brain function and neurological changes of brain or emotion disorders in children with GD type I, which will aid in the development of treatment plans for GD patients that address both physical and psychological concern and preventing neurological disease in early stage.Acknowledgements
We thank Dr. Hao Huang at University of Pennsylvania for consultation and support on MR pulse sequences.References
1. Chérin P, Rose C, de Roux-Serratrice C, et al. The neurological manifestations of Gaucher disease type 1: the French Observatoire on Gaucher disease (FROG). J Inherit Metab Dis.2010;33(4):331-338.
2. Nagral A.Gaucher disease. J Clin Exp Hepatol. 2014;4(1):37-50.
3. Wong K, Sidransky E, Verma A, et al.Neuropathology provides clues to the pathophysiology of Gaucher disease. Mol Genet Metab.2004;82(3):192-207.
4. Capablo JL, Saenz de Cabezón A, Fraile J, et al.Neurological evaluation of patients with Gaucher disease diagnosed as type 1. J Neurol Neurosurg Psychiatry.2008;79(2):219-222.
5. Giraldo P, Capablo JL, Alfonso P, et al.Neurological manifestations in patients with Gaucher disease and their relatives, it is just a coincidence? J Inherit Metab Dis.2011;34(3):781-787.
Figures

The regions with abnormal ReHo in patients(PA) with GD type I when comparing with normal controls(CN).