1621
A Prospective, Longitudinal Assessment of Adverse Local Tissue Reactions in Resurfacing Hip Arthroplasty Versus Primary Total Hip ArthroplastyMatthew F. Koff1, Owen G. Drinkwater1, Danyal G. Nawabi2, Edwin Su3, Douglas Padgett4, and Hollis G. Potter1
1Department of Radiology and Imaging, Hospital for Special Surgery, New York, NY, United States, 2Department of Orthopedic Surgery - Hip Preservation Service, Hospital for Special Surgery, New York, NY, United States, 3Department of Orthopedic Surgery - Adult Reconstruction and Joint Replacement Service, Hospital for Special Surgery, New York, NY, United States, 4Department of Orthopedic Surgery - Adult Reconstruction and Joint Replacement Service - Adult Reconstruction and Joint Replacement Service, Hospital for Special Surgery, New York, NY, United States
Synopsis
Total hip arthroplasty devices are successful achieving pain reduction, but adverse local tissue reactions (ALTRs) frequently occur for metal-on-metal hip resurfacing arthroplasty (HRA) patients. This longitudinal study evaluated if HRA patients have a greater prevalence of ALTRs as compared to ceramic-on-poly (COP) patients. Images were acquired at 2 time points, with a 1 year interval, and evaluated for synovitis and ALTR. ALTR prevalence and synovial thickness was greater in HRA than COP subjects at both time points, with significant increases at the second time point. This study will permit a better understanding of the natural history in the development of ALTR near arthroplasty.
Introduction
Over 300,000 primary total hip arthroplasty (THA) procedures were performed in 2012 (1). Many of the implants will be successful in achieving pain reduction, but adverse local tissue reactions (ALTRs) are a cause for concern in patients with metal-on-metal (MoM) total hip arthroplasty (THA) or hip resurfacing arthroplasty (HRA) devices, as well as patients with metal-on-poly modular designs (2,3). Previous studies have shown increased prevalence of ALTR with increased length of implantation in MOM THA patients (4). The purpose of this longitudinal, prospective study was to determine if patients with an HRA implant have a greater prevalence of ALTRs compared to ceramic-on-poly (COP) controls, and to assess changes in patient-reported outcomes between these two types of implant designs.Methods
Following IRB approval with informed consent, primary THA patients who were at least 1 year post-op were enrolled. A total of 69 subjects (69 hips) were evaluated at an initial time point (TP1): HRA, n=33, 9F/24M, age=54.0±6.8 y.o. (mean±SD), with length of implantation (LOI) = 4.2±2.0 yr; COP, n=36, 22F/14M, age=61.0±8.9 yr, with LOI = 3.5±3.2 yr). 53 of these subjects were evaluated at a second time point (TP2), approximately one year later: HRA, n=25; COP, n=28. Magnetic resonance imaging was performed using clinical 1.5T scanners (GE Healthcare, Waukesha, WI) and 8 channel cardiac coils (Invivo, Gainesville, FL). Morphologic and susceptibility reduced images were acquired for each hip (5,6), and were evaluated for the presence of synovitis, including synovial thickness and volume, and presence of ALTR (7). The acetabular inclination angle was calculated from radiographs. Patient-relevant outcomes were evaluated by Hip Disability and Osteoarthritis Outcome Scores (HOOS) (8). Blood samples were acquired to assess serum Cobalt and Chromium ion levels. Statistical Analysis: A Wilcoxon Rank Sum test (SAS V9.3, Cary, NC) was performed to detect differences of age, synovial thickness and volume, LOI, inclination angle, HOOS scores, and Cobalt and Chromium levels between COP and HRA subjects. Chi-squared analyses were performed to determine differences in gender distribution by implant type and to detect differences in presence of an ALTR by implant type. Spearman correlations were calculated between serum ion levels and corresponding synovial thickness and volume. Significance was set at p<0.05.Results
The HRA subjects were younger (p=0.002), had a longer LOI at TP1 (p=0.03), and were predominantly male (73%, p=0.008). The synovial thickness of the HRA and COP subjects was similar at TP1 (HRA: 3.0±2.1 mm, COP: 2.4±1.1 mm, p=0.45); however, the synovial thickness in HRA subjects was significantly larger than COP subjects at TP2 (HRA: 3.0±1.3 mm, COP: 2.1±0.8 mm, p=0.004). The prevalence of an ALTR was significantly greater in HRA than COP subjects at both time points (TP1: p=0.02, TP2:p=0.009), with an increase in the proportion of affected HRA subjects at TP2 (TP1: HRA=5/33 (15.2%), COPs =0/36 (0%); TP2: HRA=6/25 (24.0%), COP: 0/36 (0%)). HRA subjects tended to have higher HOOS scores than COP subjects at TP1 (HRA: 66.7±11.5; COP: 63.6±13.2, p=0.09), while COP subjects tended to have higher HOOS scores at TP2 (HRA:65.8±12.8; COP: 66.3±7.8, p=0.33). HRA subjects had greater Cobalt and Chromium serum ion levels than COP subjects at both time points (p<0.0001). Inclination angle did not differ by type of implant (HRA: 43.9˚±7.6˚; COP: 41.6˚ ±6.6˚ degrees; p=0.2). No significant correlations were found between Cobalt or Chromium ion levels and corresponding synovial thickness or volume.Discussion
This prospective, longitudinal study of HRA and COP subjects utilized MRI and patient reported outcome measures to evaluate synovial reactions around the implants and the subjective function of the subjects, respectively. The HRA subjects reported slightly better function than COP participants at TP1, but the results indicate that synovial thickness, the dominant MRI marker of ALTRs, was significantly greater in this cohort. These preliminary longitudinal data suggest that increased synovial thickness occurs in subjects with HRA, even while self-assessed joint function is well maintained, indicating that symptoms alone are insufficient to warrant MRI screening. MRI is a non-invasive imaging modality that is uniquely capable of detecting longitudinal differences in the peri-prosthetic soft tissues in subjects with different bearing surfaces. Our continued imaging of these patients will permit a better understanding of the natural history in the development of ALTR near arthroplasty.Conclusion
HRA patients may have adequate post-operative THA function, as compared to COP designs; however, ALTRs may develop or continue to expand, requiring the use of MRI to non-invasively monitor the surrounding soft tissues and identify premature implant failure. Neither patient reported subjective symptoms, nor serum ions levels, are capable of monitoring this process, underscoring the importance of noninvasive MR imaging.Acknowledgements
Research reported in this publication was supported by NIAMS/NIH (R01-AR064840). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.References
1. Agency for Healthcare Research and Quality. HCUPnet, Healthcare Cost and Utilization Project. https://www.hcup-us.ahrq.gov/. Accessed 29 Sept, 2016. 2. Nawabi DH, Hayter CL, Su EP, Koff MF, Perino G, Gold SL, Koch KM, Potter HG. MRI Findings in Symptomatic vs. Asymptomatic Subjects Following MOM Hip Resurfacing Arthroplasty. JBJS Am 2013;95:895-902. 3. Burge AJ, Gold SL, Lurie B, Nawabi DH, Fields KG, Koff MF, Westrich G, Potter HG. MR Imaging of Adverse Local Tissue Reactions around Rejuvenate Modular Dual-Taper Stems. Radiology 2015;277:142-150. 4. Greiner JJ, Callaghan JJ, Bedard NA, Liu SS, Goetz DD, Mahoney CR. Metal-on-Metal Total Hip Arthroplasty at Five to Twelve Years Follow-Up: A Concise Follow-Up of a Previous Report. J Arthroplasty 2016;31:1773-1778. 5. Potter HG, Nestor BJ, Sofka CM, Ho ST, Peters LE, Salvati EA. Magnetic resonance imaging after total hip arthroplasty: evaluation of periprosthetic soft tissue. JBJS Am 2004;86-A:1947-1954. 6. Koch KM, Lorbiecki JE, Hinks RS, King KF. A multispectral three-dimensional acquisition technique for imaging near metal implants. Magn Reson Med 2009;61:381-390. 7. Nawabi DH, Gold S, Lyman S, Fields K, Padgett DE, Potter HG. MRI predicts ALVAL and tissue damage in MOM hip arthroplasty. CORR 2014;472:471-481. 8. Nilsdotter AK, Lohmander LS, Klassbo M, Roos EM. Hip disability and osteoarthritis outcome score (HOOS)--validity and responsiveness in total hip replacement. BMC Musculoskelet Disord 2003;4:10.Figures
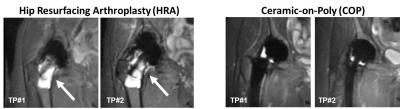
MAVRIC-SL STIR images of a patient
with an HRA implant (Left) and a patient with a COP implant (Right) evaluated
at 2 time points (TP#1, TP#2) with a 1 year interval. The HRA shows progressive
osteolysis around the femoral stem (arrow). The synovium had a 33% volumetric
increase between the time points. The COP shows a normal capsule with no
osteolysis and had a 3.4% reduction of synovial volume between the time points.