Thomas J Wilson1, Shelby A Stewart2, B. Matthew Howe3, Robert J Spinner4, and Kimberly K Amrami5
1Neurosurgery, Mayo Clinic, Rochester, MN, United States, 2Radiology, Mayo Clinic, Rochester, MN, United States, 3Radiology, Mayo Clinic, 4Neurosurgery, Mayo Clinic, Rochester, MN, 5Radiology, Mayo Clinic, Rochester, MN
Synopsis
Intraneural perineurioma is typically diagnosed
by targeted fascicular biopsy and histopathologic analysis. Through review of clinical history and
magnetic resonance imaging of consecutive patients undergoing fascicular
biopsy, we define the classical features of intraneural perineurioma as no
cancer history, unifocal disease, moderate-severe T2 hyperintensity,
moderate-severe contrast enhancement, homogeneous contrast enhancement,
fusiform shape, and enlargement of involved nerves. This combination of features has a high
specificity and moderate sensitivity for the diagnosis of perineurioma. When
the classical features of perineurioma defined in this study are present, the
high specificity of this combination of features may obviate the need for
fascicular biopsy.
PURPOSE
Intraneural perineurioma is a benign neoplasm
derived from the perineurium of peripheral nerves. Diagnosis is typically made via targeted
fascicular biopsy of the affected nerve and histopathologic analysis. The aim of the current study was to determine
if the magnetic resonance imaging (MRI) combined with the clinical features of
intraneural perineuriomas are diagnostic based on a large cohort, and second,
to determine if clinical assessment and MRI alone are sufficient for diagnosis
obviating the need for targeted fascicular biopsy.
METHODS
Consecutive patients undergoing targeted
fascicular biopsy between 2004 and 2010 were retrospectively identified. Patients with a non-diagnostic biopsy were
excluded. The MRI immediately prior to
the fascicular biopsy was reviewed for each patient. Data collected included age, sex, clinical
presentation, history of cancer, pathologic diagnosis, signal intensity on
T1-weighted, T2-weighted, and presence and pattern of enhancement on post-gadolinium
fat saturated images, shape of the lesion, uni- versus multi-focality, whether
involved nerves were enlarged, evidence of fatty muscular atrophy or subacute
denervation changes in the associated nerve territory. Pathologic diagnosis was dichotomized to
intraneural perineurioma and other. The
outcome of interest was the set of features predictive of a diagnosis of
intraneural perineurioma. Univariate
logistic regression analysis was performed to test each variable for its
ability to predict a diagnosis of perineurioma.
The rpart statistical package in R was then used to create a classification
tree for the diagnosis.
RESULTS
A total of 117 patients were included in the
study; 27 had a pathologic diagnosis of intraneural perineurioma. Factors predictive of a diagnosis of
perineurioma included moderate-severe contrast enhancement (OR 38.70, 95% CI
7.42 – 713.47, p<0.001), homogeneous contrast enhancement (OR 19.06, 95% CI
4.79 – 128.85, p<0.001), and fusiform shape (OR 4.55, 95% CI 1.22 – 29.58,
p=0.02). Factors reducing the likelihood
of a diagnosis of perineurioma included history of cancer (OR 0.05, 95% CI
0.003 – 0.23, p=0.003), presentation with pain (OR 0.23, 95% CI 0.05 – 0.71,
p=0.009), and multi-focality (OR 0.09, 95% CI 0.005 – 0.43, p=0.001). We defined the classical features of intraneural
perineurioma to be no cancer history (27/27 perineurioma group), unifocal
disease (27/27), moderate-severe T2 hyperintensity (22/27), moderate-severe
contrast enhancement (20/20 in patients in whom contrast was given),
homogeneous contrast enhancement (18/20 in patients in whom contrast was
given), fusiform shape (25/27), and enlargement of involved nerves
(27/27). Classical features were present
in 24 patients; 21 diagnosed with perineurioma and 3 with another
diagnosis. The sensitivity of the
classical features was 78% and specificity 97%.
For the 3 false positives, the actual diagnoses were traumatic neuroma,
microvasculitis, and glomangiomyoma. We
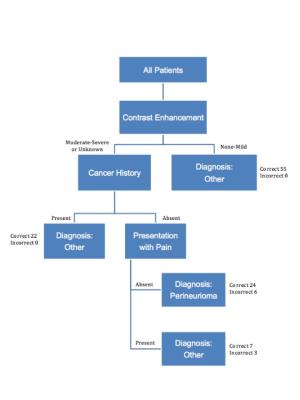
utilized R to construct a classification tree based on the rpart algorithm
(Figure 1). Features included in the
classification tree were severity of contrast enhancement, history of cancer,
and clinical presentation with pain. Sensitivity of the classification tree was
89% and specificity 93%.
DISCUSSION
Classical features of intraneural perineurioma
defined in this study included no cancer history, unifocal disease,
moderate-severe T2 hyperintensity, moderate-severe contrast enhancement,
homogeneous post-gadolinium contrast enhancement, fusiform shape, and
enlargement of involved nerves. This
combination of features had a high specificity with moderate sensitivity, and
thus is conservative as a diagnostic algorithm with few false positives. The classification tree created here had an
improved sensitivity but poorer specificity in comparison to the classical
features. In order to obviate the need
for biopsy and avoid misdiagnosis, the specificity needs to be high. The sensitivity in this case is less
important since false negatives would be captured with biopsy. As a result, the classical features
outperformed the classification tree, since the specificity was higher.
CONCLUSION
When the classical features of
perineurioma defined in this study are present, the high specificity of this
combination of features may obviate the need for fascicular biopsy and
pathologic diagnosis. Fascicular biopsy
should continue to be performed when any of the classical features are absent.
Acknowledgements
No acknowledgement found.References
No reference found.