1596
An Efficacy Analysis of Whole-Body Magnetic Resonance Imaging in the Diagnosis and Follow-Up of Polymyositis and Dermatomyositis1China-Japan Friendship Hospital, Beijing, People's Republic of China, 2Philips Healthcare (China)
Synopsis
To evaluate the value of whole-body magnetic resonance imaging (WBMRI) in diagnosing muscular and extramuscular lesions in patients with polymyositis (PM) and dermatomyositis (DM). A retrospective analysis of WBMRI data was performed on PM / DM patients who met the Bohan and Peter diagnostic criteria. WBMRI comprehensively displays the muscular involvement in PM / DM patients, and has the ability to diagnose other associated extramuscular diseases, such as ILD and systemic malignancy. WBMRI can also help screen for multifocal steroid-induced osteonecrosis.
Objectives
To evaluate the value of whole-body magnetic resonance imaging (WBMRI) in diagnosing muscular and extramuscular lesions in patients with polymyositis (PM) and dermatomyositis (DM).
Methods
A retrospective analysis of WBMRI data was performed on PM / DM patients who met the Bohan and Peter diagnostic criteria.Results
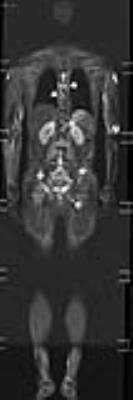
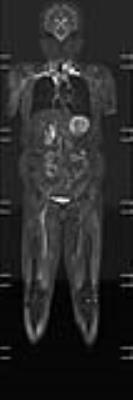
The study included 129 patients (30 PM cases and 99 DM cases). Of them, 81.4% (105/129) had a visible presence of inflammatory muscular edema on their WBMRI; 29.5% (38/129) had varying degrees of fatty infiltration (9 cases with clear muscular atrophy). Among 105 patients with inflammatory muscular edema, the most frequently affected area was the thigh muscle, present in 99.0% (104/105) cases. In 35.2% (37/105) patients, the thigh muscle had less severe edema than other parts of the body (Figure 1). WBMRI showed ILD in 29.5% (38/129) of patients (Fig. 2, 3). The prevalence of ILD was 33.3% (33/99) and 16.7% (5/30) in DM and PM patients respectively. A WBMRI detected osteonecrosis in 15 patients. Thirty-eight joints were affected (mean, 2.5 per patient; range, 1–5 joints). The hip was the most often affected(19 hips, 11 patients) (Figure 2), followed by the knee (13 knees in 7 patients) (Fig. 3), shoulder (3 shoulders in 2 patients), and ankle (3 ankles in 2 patients). Of the 38 joints affected by osteonecrosis, 33 had no clinical symptoms. In addition, WBMRI discovered tumors in 12 patients (9.3%). Five were later diagnosed as malignant and seven were diagnosed with benign tumors. Five malignant tumors included cervical lymph node and/or multiple bone metastasis of nasopharyngeal carcinoma (3 cases)(Fig. 4), thyroid cancer (1 case) (Fig. 5), and liver metastasis after ovarian cancer had been surgical resection (1 case).Discussion
Polymyositis (PM) and dermatomyositis (DM) fall into the class of idiopathic inflammatory myopathies, a group of autoimmune diseases characterized by inflammatory changes of the skeletal muscle [1]. Although muscular and skin changes are characteristic presentations, PM / DM is a systemic disease. Lungs are the second most involved organ after the skin and muscular system. Interstitial lung disease (ILD) is the most frequent manifestation, reported in up to 35-40% of DM patients [2]. Meanwhile, a considerable proportion of PM / DM patients also report malignance. ILD and cancer are important factors affecting the prognosis of PM / DM patients [2]. Furthermore, glucocorticoids are the preferred treatment for PM / DM patients, but are also the primary cause of non-traumatic osteonecrosis [3]. In recent years, there have been reports that demonstrate the success of whole-body magnetic resonance imaging (WBMRI) through short tau inversion recovery (STIR) sequence in the diagnosis of PM / DM [4-6]. A WBMRI scan covers the whole body, but its value in the diagnosis of ILD, cancer and other PM / DM associated extramuscular lesions remains unclear.
This study shows that although thigh musculature is the most frequently involved in PM / DM patients, the edema is less severe than other affected muscles of the bodies in about 1/3 patients, indicating that muscular inflammation in PM / DM patients is often uneven distribution, and that relying on MRI findings of thigh muscles alone may lead to misjudgement. In addition to muscular changes, WBMRI also detected interstitial lung disease (ILD) in 38 cases (29.5%), osteonecrosis in 15 cases (11.6%), and neoplastic lesions (5 malignant; 7 benign) in 12 cases (9.3%). Because of the close relationship between DM / PM and malignancy, DM / PM patients with risk factors should be promptly screened for cancer. The assessment of WBMRI in screening malignant tumors in patients with PM / DM has not been reported before. the use of a WBMRI in the diagnosis of osteonecrosis in PM / DM patients was also limited to the reporting from individual cases [7].
Conclusions
WBMRI is a sensitive, non-invasive and efficient imaging method. It can provide a comprehensive assessment of muscular involvement in PM / DM patient cases, detect PM/DM associated extramuscular diseases such as ILD and systemic malignancy, and help screen for steroid-induced osteonecrosis. Thus, it should be considered as a promising examination for PM / DM diagnosis and follow-up.Acknowledgements
References
1.Dalakas MC, Hohlfeld R (2003) Polymyositis and dermatomyositis. Lancet 362:971-82.
2. Marvi U, Chung L, Fiorentino DF (2012) Clinical presentation and evaluation of dermatomyositis. Indian J Dermatol 57:375-81.
3. Malizos KN, Karantanas AH, Varitimidis SE, Dailiana ZH, Bargiotas K, Maris T (2007) Osteonecrosis of the femoral head: etiology, imaging and treatment. Eur J Radiol 63:16-28.
4. Cantwell C, Ryan M, O'Connell M, et al (2005) A comparison of inflammatory myopathies at whole-body turbo STIR MRI. Clin Radiol 60:261-7.
5. Ley S, Ley-Zaporozhan J, Schenk JP (2009) Whole-body MRI in the pediatric patient. Eur J Radiol 3:442-51.
6. O'Connell MJ, Powell T, Brennan D, Lynch T, McCarthy CJ, Eustace SJ (2002) Whole-body MR imaging in the diagnosis of polymyositis. AJR Am J Roentgenol 174:967-71
7. Castro TC, Lederman H, Terreri MT, Kaste SC, Hilario MO (2010) Detection of multifocal osteonecrosis in an adolescent with dermatomyositis using whole-body MRI. Pediatr Radiol 40:1566-8.
8. Miller SA, Glassberg MK, Ascherman DP (2015) Pulmonary complications of inflammatory myopathy. Rheum Dis Clin North Am 41:249-62.
9. Taborda AL, Azevedo P, Isenberg DA (2014) Retrospective analysis of the outcome of patients with idiopathic inflammatory myopathy: a long-term follow-up study. Clin Exp Rheumatol 32:188-93.
10. Hallowell RW, Ascherman DP, Danoff SK (2014) Pulmonary manifestations of polymyositis/dermatomyositis. Semin Respir Crit Care Med 35:239-48.
11. Chen D, Yuan S, Wu X, et al (2014) Incidence and predictive factors for malignancies with dermatomyositis: a cohort from southern China. Clin Exp Rheumatol 32:615-21.
12. Shah AA, Casciola-Rosen L, Rosen A (2015) Review: cancer-induced autoimmunity in the rheumatic diseases. Arthritis Rheumatol 67:317-26.
13. Wang J, Guo G, Chen G, Wu B, Lu L, Bao L (2013) Meta-analysis of the association of dermatomyositis and polymyositis with cancer. Br J Dermatol 169:838-47.
14. Zalavras CG, Lieberman JR (2014) Osteonecrosis of the femoral head: evaluation and treatment. J Am Acad Orthop Surg 22:455-64.
15. Karantanas AH (2013) Accuracy and limitations of diagnostic methods for avascular necrosis of the hip. Expert Opin Med Diagn 7:179-87.
16. Mitchell MD, Kundel HL, Steinberg ME, Kressel HY, Alavi A, Axel L (1986) Avascular necrosis of the hip: comparison of MR, CT, and scintigraphy. AJR Am J Roentgenol 147:67-71.
17. Karantanas AH, Drakonaki EE (2011) The role of MR imaging in avascular necrosis of the femoral head. Semin Musculoskelet Radiol 15:281-300.
18 Zibis AH, Karantanas AH, Roidis NT, et al (2007) The role of MR imaging in staging femoral head osteonecrosis. Eur J Radiol 63:3-9.
Figures