1590
Potential of High Resolution Isotropic Microstructural MRI of the Proximal Femur1University of Pennsylvania, Philadelphia, PA, United States, 2University of Pennsylvania, 3New York University
Synopsis
Microstructural MRI based finite element modelling is an area of current research in regards to the role that this technology can play as an efficient and affordable metric for quantifying bone integrity and for identifying fracture risk. This study was conducted in an attempt to unveil the extent to which MRI resolution impacts the quantitative output generated by finite element models pertaining to the parameter of bone stiffness of the proximal femur in vitro. Conclusions reveal a statistically significant variance relative to the values generated for two differing MRI resolution classes.
Purpose
Microstructural MRI based finite element modelling has been presented as a viable and reproducible means to assess bone quality and identify patients at risk for hip fracture1. Recently demonstrated microstructural hip MRI sequences use higher resolution in coronal plane while relaxing the slice resolution (0.5-1.5 mm) to avoid long scan time.2-3 However, use of anisotropic resolution is not optimal for MRI-based finite element modeling of the proximal femur because the trabeculae are not aligned in one direction as in distal extremities. The aim of this study was to investigate the feasibility of using an isotropic high-resolution MRI sequence for generating finite element models of the hip.Methods
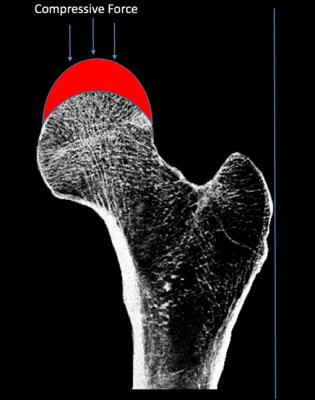
Seven human cadaveric proximal femurs were selected for study and harvested from four female and three male specimens, ranging in age from 36-88 years. Bone specimens were imaged on a 3 Tesla whole body clinical MRI scanner (Siemens Prisma, Erlangen, Germany) incorporating an 18-element receive-coil using two different protocols: (1) bSSFP sequence with 0.3-mm isotropic voxel size and (2) previously developed FLASH sequence with 0.242 mm x 0.242 mm x 1.5 mm voxel size.1,3 Bone volume fraction maps were generated on the basis of these images by linear scaling of image grayscale values ranging from 0% (completely marrow) to 100% (completely bone). Finite element models were generated as previously described by converting voxels in the bone volume fraction map to a finite element mesh.1,3 Bone stiffness was computed by simulating stance loading conditions by applying displacement to the femoral head through a consistent geometric configuration that sought to mimic the native acetabular architecture.Results
Donor age was inversely correlated with stiffness derived from the isotropic (R2=0.84) and anisotropic resolution (R2=0.68) images. Furthermore, stiffness derived from the isotropic and anisotropic resolution images were highly correlated (R2=0.96).Discussion
The determination of inversely correlated bone stiffness and donor age variables for both of the MRI resolution classes represents a logical conclusion as aging is accompanied by bone deterioration resulting in a decline in bone’s mechanical integrity. The disparity between the correlation values determined for the two varying resolution classes is a significant finding as it supports the sentiment that MRI resolution has a profound impact on the values generated by finite element models. Furthermore, the higher correlation value generated by analysis using the segmented images of the 300 micrometer isotropic resolution support the assertion that higher quality MRI images could contribute to more accurate finite element models for predicting bone stiffness. This is due in part to the introduction of potential inaccuracies in the application of the finite element mesh on lower resolution MRI images as a consequence of the fact that the trabeculae are not sufficiently resolved due to the multi-dimensional orientation at the proximal femur.Conclusion
Further studies are needed to determine if higher resolution finite element models could estimate proximal femur mechanical properties compared to currently used anisotropic models and compared to direct mechanical testing of cadaveric bone.Acknowledgements
No acknowledgement found.References
1. Rajapakse CS, Hotca A, Newman BT, Ramme A, Vira S, Kobe EA, Miller R, Honig S, Chang G. Patient specific hip strength and fracture risk assessment by microstructural mri-based finite element modeling. Radiology. (in press).
2. Han M, Chiba K, Banerjee S, Carballido-Gamio J, Krug R. Variable flip angle three-dimensional fast spin-echo sequence combined with outer volume suppression for imaging trabecular bone structure of the proximal femur. J Magn Reson Imaging. 2015 May;41(5):1300-10.
3. Chang G, Honig S, Brown R, Deniz CM, Egol KA, Babb JS, Regatte RR, Rajapakse CS. Finite element analysis applied to 3-T MR imaging of proximal femur microarchitecture: lower bone strength in patients with fragility fractures compared with control subjects. Radiology. 2014 Aug;272(2):464-74.