1583
Analysis of T2 Relaxation Times in Vastus Lateralis Muscle after Anterior Cruciate Ligament Injury1College of Engineering, Department of Biomedical Engineering, Lexington, KY, United States, 2Department of Radiology, College of Medicine, Lexington, KY, United States, 3Magnetic Resonance Imaging and Spectroscopy Center, Lexington, KY, United States, 4Department of Neuroscience, College of Medicine, 5Department of Rehabilitation, College of Health Sciences, Lexington, KY, United States
Synopsis
Anterior cruciate ligament (ACL) injuries are associated with a persistent decrease in quadriceps muscle strength despite rehabilitation. Previous studies have shown that ACL injury results in muscle disorganization, which could account for the loss in strength. We sought to use dual-spin echo and multi-spin echo sequences to estimate T2 of the vastus lateralis in injured and uninjured limbs of twenty-two ACL injured subjects. T2 of the injured limb was significantly longer than the uninjured limb for both pulse sequences. Our results suggest that T2 relaxation may provide clinicians a means to quantitatively monitor muscle recovery after ACL injury.
Introduction
ACL injuries are among the most common sports related injuries in the United States.1 Despite extensive rehabilitation, an ACL injury has been shown to result in a persistent decrease in quadriceps muscle strength as well as changes in muscle morphology. Among these changes is an expansion of the extracellular matrix and an increase in the collagen content around the muscle fibers.2 We sought to measure the changes in T2 estimated from dual spin echo (DSE) and multi spin echo (MSE) MRI to quantitatively assess changes in the vastus lateralis (VL) after tearing and reconstruction of the ACL. The MSE sequence produces more echoes and may give a more accurate estimation of the T2. The DSE sequence is faster and therefore can acquire a greater volume of the VL in a given acquisition time. If the two techniques produce equivalent results the increased acquisition efficiency of the DSE may be preferable in clinical practice. We hypothesized that ACL injury results in longer T2 of the quadriceps muscles of the injured limb when compared to the contralateral limb for both the DSE and MSE pulse sequences.Methods
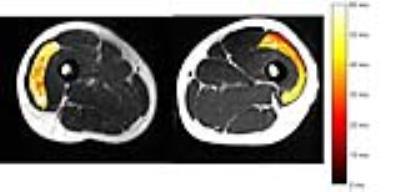
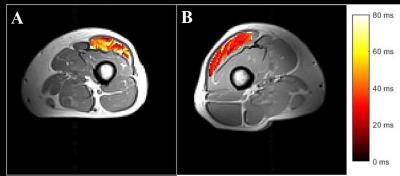
Twenty-two subjects (16M, 6F, 24±5 years old) who had either an ACL injury or ACL reconstruction volunteered to participate in the study. All imaging was performed on a 3.0 T, Siemens MAGNETOM Tim Trio scanner. Signal was received through a multi-element, flexible, body array coil positioned directly over the subject’s VL. A turbo spin echo sequence was used to acquire axial DSE (Figure 1) and MSE (Figure 2) MR images over the length of the VL. Specific parameters for the DSE pulse sequence include TE = 12/71ms, TR = 4210ms, spatial resolution = 1.53mm x 1.53mm, slice thickness = 6mm, matrix = 256 x 128. Specific parameters for the MSE pulse sequence include ten equi-spaced echoes from TE = 13.1-131.0ms, TR = 3000ms, spatial resolution = 1.53mm x 1.53mm, slice thickness = 6mm with a 6mm gap, matrix = 128 x 128. Nineteen subjects received the DSE pulse sequence and eight subjects received the MSE pulse sequence and five subjects received both pulses. Approximately ten mid-muscle slices per leg on each individual were chosen for analysis based on muscle thickness. All data analysis was performed in Matlab (Mathworks, Nattick, MA). T2 relaxation was estimated using non-linear, least squares regression. In the case of the MSE images we excluded the first echo from the decay analysis because of the different stimulated echo weighting of this image compared to the later echo images.Results
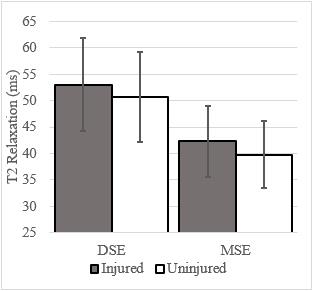
T2 relaxation time of the VL was increased in the injured limb in sixteen out of the twenty-two subjects. Using independent t-tests, a significant increase in the mean T2 relaxation for the injured limb was found in both the DSE (p=0.01) and MSE (p=0.03) scans (Figure 3). A repeated measures ANOVA showed significance with leg as the within-subjects factor (p=0.001) and method as the grouping factor (p<<0.001). T2 relaxation times for DSE were, on average, 11ms higher than T2 estimated from MSE.Discussion/Conclusion
Our results suggest that T2 weighted imaging is sensitive to the changes in quadriceps muscles resulting from ACL injury. T2 measured in the VL using either DSE or MSE techniques demonstrated significant increase in the ACL injured limb. We hypothesize the increase in T2 results from increased fluid accumulation as a consequence of the development of fibrosis in the extracellular matrix of the muscle. The MSE T2 measurements were closer to results reported by other groups3,4 than the measurements from the DSE scans. Additionally, the variation from subject to subject was lower in the MSE sequence. On the other hand, the DSE sequence acquired more slices in a shorter time. The absence of an interaction effect between image acquisition methods suggests they are consistent in their ability to distinguish the injured and uninjured limbs. Our results show that DSE may provide clinicians a useful and rapid means to estimate T2 in order to identify changes to muscle organization after ACL injury.Acknowledgements
Research reported in the publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health through award number K23AR062069.References
1. Mather, I.I.I.R.C., et al., Societal and Economic Impact of Anterior Cruciate Ligament Tears. The Journal of Bone & Joint Surgery, 2013. 95(19): p. 1751-1759.
2. Hasson, C. J., et al. Contractile and non-contractile tissue volume and distribution in ankle muscles of young and older adults. J Biomech, 2011 44(12): p. 2299-2306.
3. Chang G., et al. Biochemical and Physiological MR Imaging of Skeletal Muscle at 7 Tesla and Above. Seminars in musculoskeletal radiology. 2010 14(2).
4. Arpan, I., et al., T2 mapping provides multiple approaches to characterize muscle involvement in neuromuscular diseases: a cross-sectional study of lower leg muscles in 5-15 year old boys with Duchenne Muscular Dystrophy. NMR Biomed., 2013 26(3): p. 320-328.
Figures