1543
T2-mapping evaluation of talar cartilage for chronic lateral ankle instability (LAI) with isolated anterior talofibular ligament (ATFL) tear, and combined ATFL and calcaneofibular ligament (CFL) tearHongyue Tao1, Yang Qiao1, Yiwen Hu1, Xu Yan2, Kui Ma3, Yinghui Hua3, and Shuang Chen1
1Department of Radiology, Fudan University Affiliated Huashan Hospital, Shanghai, People's Republic of China, 2MR Collaboration NE Asia, Siemens Healthcare, Shanghai, People's Republic of China, 3Department of Sports Medicine, Fudan University Affiliated Huashan Hospital, Shanghai, People's Republic of China
Synopsis
The study aimed to use T2-mapping to quantitatively evaluate talus cartilage for chronic lateral ankle instability (LAI) with isolated anterior talofibular ligament (ATFL) tear, and combined ATFL and calcaneofibular ligament (CFL) tear. Seventeen patients with ATFL tear, 10 with ATFL+CFL tear, and 21 healthy subjects were recruited. All participants underwent T2-mapping scan, and patients completed American-Orthopedic-Foot-and-Ankle-Society (AOFAS) scoring. The results indicated that chronic LAI with ATFL+ CFL tear may result in much larger and more severe cartilage degeneration than isolated ATFL tear, and medial anterior of talus could be the main cartilage compartment affecting patients’ clinical symptom and prognosis.
Purpose
The
lateral ankle ligament complex consists of three major ligaments: anterior
talofibular ligament (ATFL), calcaneofibular ligament (CFL), and posterior
talofibular ligament (PTFL)1. ATFL injury occurs most frequently and
is thus of high clinical importance, followed by combined injury of ATFL and
CFL2. 10%–30% of patients with repeat ankle sprains may develop into
chronic lateral ankle instability (LAI)1. Chronic LAI altered
tibiotalar kinematics, which has been suggested to contribute to the
development of chondral lesions and the progress of osteoarthritis (OA)3.
Previous studies mainly focused on the cartilage change resulting from isolated
ATFL injury. However, there are limited data on the cartilage alteration of combined
ATFL and CFL tear. Therefore, the purpose of this study was to quantitatively
evaluate the cartilage alteration of talus for chronic LAI with isolated ATFL
tear and combined ATFL and CFL tear using T2-mapping, which is a very powerful
tool for noninvasive assessment of biochemical changes in the cartilage matrix
that precede morphological deterioration4, and analyze the
correlation between T2 value and AOFAS score.Methods
A total of 27 patients and 21 healthy controls were included in this study. Patients were divided into two groups: 1) ATFL group, 17 patients with ATFL tear; 2) ATFL+CFL group, 10 patients with combined ATFL and CFL tear. MRI examinations were performed on a 3T scanner(MAGNETOM Verio, Siemens Healthcare, Erlangen, Germany) with a gradient strength of 45mT/m using an 8-channel phased array coil. The MR imaging sequences and parameters are displayed in Table 1. T2 maps and AOFAS scores were acquired for all patients. The total talar trochlear cartilage (TTC) was manually segmented into six compartments by two radiologists: medial anterior (MA), medial center (MC), medial posterior (MP), lateral anterior (LA), lateral center (LC), and lateral posterior (LP), and the T2 value of each compartment was measured from the T2-mapping images. Then, the color-scale T2-mapping images were fused with T2-weighted images to reflect the detailed topographic distribution of T2 value using a MRWP workstation (Siemens Healthcare, Erlangen, Germany). Data were analyzed with one-way analysis of variance (ANOVA), Student's t-test and Pearson's correlation coefficient. Statistical significance was defined with P<0.05.Results
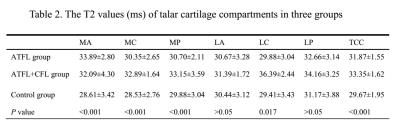
There were no significant differences in age, sex or BMI between patients and control subjects. The T2 values of MA, MC, MP, LC cartilage compartments and TTC were significantly different among the ATFL, ATFL+CFL and control group (Table 2). More specifically, the T2 values of the ATFL group were significantly higher than those of controls in MA, MC, MP cartilage compartments and TTC (P<0.001, P=0.033, P=0.003, P<0.001, respectively) (Fig.1, Fig. 2. A). The T2 values of the ATFL+CFL group were significantly higher than those of controls in MA, MC, MP, LC, LP cartilage compartments and TTC (P=0.011, P=0.001, P<0.001, P=0.005, P=0.032, P<0.001, respectively) (Fig.1, Fig. 2. B). Moreover, the T2 values of the ATFL+CFL group were higher than those of the ATFL group in MC, MP, LC cartilage compartments and TTC (P=0.016, P=0.017, P=0.037, P=0.04, respectively) (Fig.1, Fig. 2. C). The AOFAS score of the ATFL+CFL group was significantly lower than those of the ATFL group (57.50±5.06 vs 70.71±6.19, P<0.001). The T2 values of MA compartment in ATFL and ATFL+CFL groups were negatively correlated with AOFAS scores (r=-0.596, P=0.012; r=-0.690, P=0.027, respectively), while no statistically significant correlations were found between T2 values of other cartilage compartments and AOFAS scores (P>0.05).Discussion and Conclusion
Chronic LAI with isolated ATFL tear may be connected to the occurrence of cartilage degeneration in talus trochlea, mainly involving medial cartilage compartments. This finding is consistent with previous studies using finite element analysis5,6, which indicated that the increased anterior translation and internal rotation of the talus may lead to increased abutment and stress distribution on the medial cartilage compartment of the talus. Besides, the combined ATFL and CFL tear may result in much larger and more severe cartilage degeneration than isolated ATFL tear. The CFL is injured by more severe inversion stress than ATFL. When the ATFL and CFL were damaged, significant increases in inversion and supination have been observed compared to isolated ATFL7,8. Additionally, MA is the main cartilage compartment which may affect the patient’s clinical symptom and prognosis. This finding may suggest that the monitoring of MA is important for chronic LAI patients, and the degeneration of MA should require early intervention in order to improve the patient’s clinical symptoms and prognosis. Finally, MRI T2-mapping can play a major role in detecting cartilage degeneration at an early stage to help plan treatment and monitor disease progression for chronic LAI.Acknowledgements
No acknowledgement found.References
1. Burks RT, Morgan J. Anatomy of the lateral ankle ligaments. Am J Sports Med 1994;22(1):72-7. 2. Baumhauer JF, O'Brien T. Surgical Considerations in the Treatment of Ankle Instability. J Athl Train 2002;37(4):458-62. 3. Valderrabano V, Hintermann B, Horisberger M, et al. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med 2006;34(4):612-20. 4. Tao H, Shang X, Lu R, et al. Quantitative magnetic resonance imaging (MRI) evaluation of cartilage repair after microfracture (MF) treatment for adult unstable osteochondritis dissecans (OCD) in the ankle: correlations with clinical outcome. EUR RADIOL 2014;24(8):1758-67. 5. Caputo AM, Lee JY, Spritzer CE, et al. In vivo kinematics of the tibiotalar joint after lateral ankle instability. Am J Sports Med 2009;37(11):2241-8. 6. Ringleb SI, Udupa JK, Siegler S, et al. The effect of ankle ligament damage and surgical reconstructions on the mechanics of the ankle and subtalar joints revealed by three-dimensional stress MRI. J ORTHOP RES 2005;23(4):743-9. 7. Fujii T, Kitaoka HB, Watanabe K, et al. Ankle stability in simulated lateral ankle ligament injuries. FOOT ANKLE INT 2010;31(6):531-7. 8. Choisne J, Ringleb SI, Samaan MA, et al. Influence of kinematic analysis methods on detecting ankle and subtalar joint instability. J BIOMECH 2012;45(1):46-52.Figures
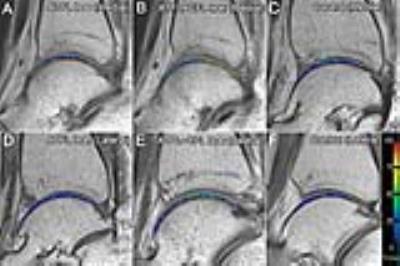
Fig. 1 The
color-scale T2-mapping images of medial cartilage of talus (A, B, C) and
lateral talus (D, E, F) of a chronic LAI patient with isolated ATFL tear (A and
D), a chronic LAI patient with ATFL+CFL tear (B and E) and a healthy control (C
and F). The T2 values of medial talus of both patients were higher than control
according to the responding color bar on the right; The T2 values of MC and MP
of ATFL+CFL tear patient were higher than ATFL tear patient. The T2 value of
lateral talus of ATFL tear patient was similar with control, while The T2 value
of LC of ATFL+CFL tear patient was higher than ATFL tear patient and control.

Fig. 2 T2 values differences in each compartment. (A) For the ATFL
group, the T2 values in MA, MC, MP cartilage compartments (blue regions) and
TTC were higher than in the control group. (B) For ATFL+CFL group, the T2
values in MA, MC, MP, LC, LP cartilage compartments (blue regions) and TTC were
higher than in the control group. (C) MC, MP and LC cartilage compartments
(blue regions) and TTC in the ATFL+CFL group with higher T2 values than in the
ATFL group.
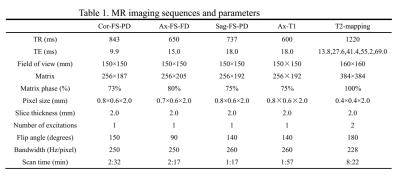
Table 1. MR imaging sequences and parameters
Table
2. The T2 values (ms) of talar cartilage compartments in three groups