1477
Respiratory Self-Gating using Principal Component Analysis in 2D Golden Angle Radial Free Breathing Cine Imaging1Department of Molecular Medicine and Surgery, Karolinska Institutet, Stockholm, Sweden, 2Department of Clinical Physiology, Karolinska University Hospital, Stockholm, Sweden
Synopsis
Due to respiratory motion, cardiac imaging is performed during breath holding. Breath holding can be strenuous, or even impossible, for patients with heart disease. We suggest a method for respiratory self-gating using a Golden Angle radial k-space trajectory and principal component analysis. Radial trajectories sample the middle of k-space, which corresponds to the large structure content of the image, each repetition time. The respiratory motion can be detected from the
Purpose
Breath holding in cardiovascular magnetic resonance (CMR) allows for imaging the heart in a constant position over several cardiac cycles, thereby achieving high spatial resolution while limiting motion artifacts. However, breath holding is difficult for the patients to perform consistently, which often results in various image artifacts that potentially could be avoided by free breathing CMR combined with retrospective respiratory gating. Detection of the respiratory motion is routinely done in the clinic with bellows, but only provides an indirect measure of the respiratory motion which is not optimal for respiratory gating.1 The purpose of the study was therefore to develop a robust free-breathing respiratory self-gating method derived directly from k-space data itself. By treating the self-gating signal as an analytical function, inspiration can be distinguished from expiration. Studies suggest that the left ventricular end diastolic volume will differ in between inspiration and expiration.2Methods
To evaluate the consitency of the proposed technique for CMR, a complete left ventricular stack of 2D short axis slices (11±1 slices, slice thickness 8 mm, distance factor 20%) was acquired during free breathing in healthy volunteers (n = 8, age 29 ± 5 years, 63% male) using radial balanced steady state free precession with golden angle ordering (flip angle 65 degrees, TR 3.2 ms, resolution 1.5x1.5 mm, 6667 radial spokes per slice). ECG and respiratory bellows signals were simultaneously acquired. The respiratory gating signal was estimated using the DC term of each radial spoke per coil element. Principal component decomposition was performed along the temporal dimension of this k-space center signal. The Fourier transform of the resulting components, which contained the most prominent peak in the range 0.1 to 0.5 Hz was selected and smoothed with a single-sided bandpass filter. The analytical representation $$$f_A$$$ of the real-valued function $$$f$$$ is defined as$$f_A = f - i\mathcal{H}(f)$$where $$$\mathcal{H}(f)$$$ denotes the Hilbert transform of $$$f$$$. It can easily be shown that nulling all negative frequencies will results in an analytical representation, thus applying a single-sided bandpass filter will result in an analytical representation of the respiratory signal. Importantly, the argument of the analytical signal describes the instantaneous phase of the respiration, thus inspiration could easily be distinguished from expiration. The duration of each respiratory cycle was measured for both the bellows and the derived respiratory gating signal by identifying the peaks of the two curves and measuring the peak-to-peak distance. An image was also reconstructed in end-diastole both with and without respiratory self-gating in end-expiration for comparison of image quality.
Results
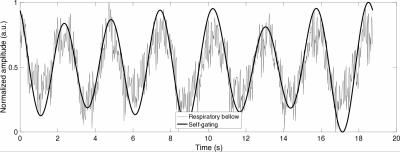
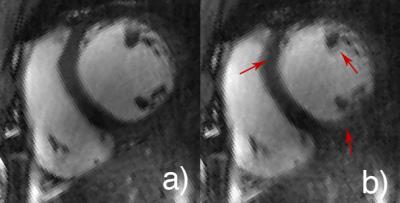
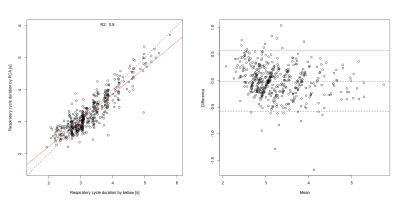
Figure 1 shows the derived respiratory self-gating signal superimposed over the measured bellows signal for a single representative slice. Figure 2 shows the reconstructed images with (a) and without (b) respiratory self-gating. Figure 3 shows the correlation between measurements of respiratory cycle duration for the two methods (n = 483 respiratory cycles, R2 = 0.80, p < 0.001, mean±SD difference 10±295 ms).Discussion
Respiratory bellows only can provide an indirect measure of respiratory phase, and is thus problematic to use as a ground truth for comparison. Previous studies comparing navigator based gating with respiratory bellows observe a phase-shift between the two methods.1 A similar phase-shift was observed in some, but not all slices in this study. The correlation between the external measurement (bellows) and the data based method is also similar to what has previously been reported in the literature.Conclusions
A robust method is presented for respiratory self-gating in 2D golden-angle radial cine imaging. The proposed method for respiratory self-gating was consistently able to detect a principal component that exhibited a strong correlation with the bellows signal. Future work will focus on validating the accuracy of the proposed method from respiratory gating and further explore its possibilities for cardiac gating.Acknowledgements
No acknowledgement found.References
1. Santelli C, Nezafat R, Goddu B, et al. Respiratory bellows revisited for motion compensation: preliminary experience for cardiovascular MR. Magn Reson Med. 2011;65(4):1097-1102.
2. Holst K, Ugander M, Sigfridsson A. Respiratory Resolved Cardiac Cine Imaging using Self-Gated Golden Angle Radial Acquisition. Proc. Intl. Soc. Mag. Reson. Med. 23. 2015
Figures