1363
Early changes of irradiated parotid glands evaluated by T1rho-weighted imaging: a pilot study1Department of Radiology, Drum Tower Hospital, School of Medicine, Nanjing University, Nanjing, People's Republic of China, 2Department of Radiology, Drum Tower Hospital, School of Medicine, Nanjing University, 3Philips Healthcare, Shanghai, People's Republic of China
Synopsis
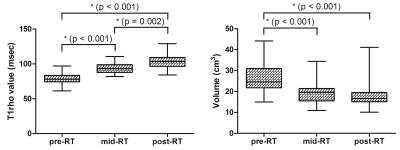
Twenty-six NPC patients underwent serial T1rho-weighted imaging to evaluate the dynamic changes of parotid glands in patients undergoing intensity-modulated radiation therapy. Parotid volumes, T1rho values, mean radiation doses, and xerostomia degrees were recorded. Change rates of T1rho values were correlated with atrophy rates, mean radiation doses and xerostomia degrees. During RT, parotid volume decreased and parotid T1rho values increased significantly. The change rate of T1rho value correlated with the atrophy rate significantly at post-RT. Intra- and interobserver reproducibility of T1rho measurements were excellent. Dynamic changes of radiation-induced parotid damage in NPC patients underwent IMRT could be evaluated by T1rho-weighted imaging.
PURPOSE
To confirm the feasibility of T1rho-weighted imaging to evaluate the dynamic changes of parotid glands in patients with nasopharyngeal carcinoma (NPC) undergoing intensity-modulated radiation therapy (IMRT).METHODS
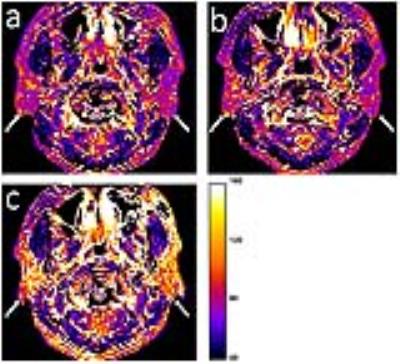
Twenty-six NPC patients (19 men, 7 women; age, 48.9 ± 13.4 years) underwent three serial T1rho-weighted imaging: within 2 weeks before radiotherapy (RT) (pre-RT), 5 weeks after the beginning of RT (mid-RT) and 4 weeks after RT (post-RT). Parotid volumes, T1rho values, mean radiation doses, and xerostomia degrees were recorded. Change rates of parotid T1rho values were correlated with parotid atrophy rates, mean radiation doses and xerostomia degrees.RESULTS
During RT, parotid volume decreased (atrophy rate, 32.7 ± 8.1% at mid-RT and 27.9 ± 10.0% at post-RT compared to pre-RT; both P < 0.001) and parotid T1rho values increased (change rate, 25.0 ± 15.8% at mid-RT and 30.1 ± 18.0% at post-RT compared to pre-RT, both P < 0.001) significantly. The change rate of parotid T1rho value correlated with the atrophy rate significantly at post-RT (r = 0.301; P = 0.047). Intra- and interobserver reproducibility of parotid T1rho measurements were excellent (intraclass correlation coefficient: 0.974 and 0.956, respectively).DISCUSSION
We found that the parotid T1rho values increased significantly during the whole course of RT, which might reflect a continuous accumulation of the extracellular matrix proteins during RT, forming the so-called “fibrosis”. A series of studies have proved the correlation between T1rho values and the fibrosis degrees of multiple tissues. Meanwhile, a significant positive correlation between the change rate of parotid T1rho values and the parotid atrophy rate at post-RT. We speculated that with the loss of parotid acinar cells, the extracellular space enlarged, accompanied with more accumulation of extracellular matrix proteins.CONCLUSION
Dynamic changes of radiation-induced parotid damage in NPC patients underwent IMRT could be noninvasively evaluated by T1rho-weighted imaging.Acknowledgements
No acknowledgement found.References
1. Kam MK, Leung SF, Zee B, et al. Prospective randomized study of intensity-modulated radiotherapy on salivary gland function in early-stage nasopharyngeal carcinoma patients. J Clin Oncol.2007;25:4873-4879.
2. Houweling AC, Schakel T, van den Berg CA, et al. MRI to quantify early radiation-induced changes in the salivary glands. Radiother and Oncol.2011;100:386-389.
3. Marzi S, Forina C, Marucci L, et al. Early radiation-induced changes evaluated by intravoxel incoherent motion in the major salivary glands. J Magn Reson Imaging.2015;41:974-982.
4. Juan CJ, Cheng CC, Chiu SC, et al. Temporal evolution of parotid volume and parotid apparent diffusion coefficient in nasopharyngeal carcinoma patients treated by intensity-modulated radiotherapy investigated by magnetic resonance imaging: a pilot study. PLoS One.2015;10:e137073.
5. Yang Q, Yu T, Yun S, et al. Comparison of multislice breath-hold and 3D respiratory triggered T1ρ imaging of liver in healthy volunteers and liver cirrhosis patients in 3.0 T MRI. J Magn Reson Imaging.2016;doi: 10.1002/jmri.25253.
Figures