1341
Preliminary Clinical Experience with FDG-PET/MRI in Plasma Cell DyscrasiasTyler J Fraum1, Daniel R Ludwig1, Ephraim E Parent1, Farrokh Dehdashti1, Michelle Miller-Thomas1, Monica Shokeen1, Keith Stockerl-Goldstein1, Ravi Vij1, and Kathryn J Fowler 1
1Mallinckrodt Institute of Radiology, Washington University School of Medicine, St Louis, MO, United States
Synopsis
Multiple
Purpose
By combining the metabolic information of PET with the high soft tissue contrast of MRI, PET/MRI, most often performed with the glucose analogue [18F]fluorodeoxyglucose (FDG), has emerged as a powerful hybrid imaging modality for various oncologic conditions. Multiple myeloma (MM) is an attractive target for FDG-PET/MRI, as both MRI and FDG-PET/CT, when performed separately, have important limitations. For example, diffuse tracer uptake by normal marrow can obscure focal myeloma lesions on FDG-PET, especially in patients receiving marrow-stimulating agents,1 while the correlative CT images are less sensitive than MRI for detecting marrow infiltration.2 On the other hand, abnormal marrow signal on MRI can persist despite clinical evidence of disease remission, while the resolution of FDG uptake by focal myeloma lesions closely correlates with clinical metrics of treatment response.3 Thus, FDG-PET/MRI, by interrogating both lesion metabolism and marrow replacement, has the potential to serve as a comprehensive imaging tool for MM and other plasma cell dyscrasias (PCDs). In this study, we provide an account of our preliminary experience with FDG-PET/MRI for PCDs at a large academic center.Methods
Since 2012, 36 patients with clinical diagnoses of MM, smoldering MM (SMM), or monoclonal gammopathy of undetermined significance (MGUS) have undergone FDG-PET/MRI at our institution. Fourteen were imaged with both PET/CT and PET/MRI on the same day as part of a PET/MRI optimization research protocol, while 22 underwent PET/MRI as part of their routine clinical care. All PET/MRI acquisitions were performed with an integrated Siemens Biograph mMR, while PET/CT was performed on a Siemens Biograph 40 or mCT. Our PET/MRI myeloma protocol, which extends from skull vertex to knees, generally included two-point Dixon images for attenuation correction, transaxial T2-weighted images (T2WIs), sagittal (spine only) and transaxial (pelvis only) turbo spin echo (TSE) T1-weighted images (T1WIs), and transaxial post-contrast T1WIs. PET/MRI studies were interpreted jointly by a nuclear medicine physician and a radiologist specializing in MRI. Patient characteristics, clinical scenarios, and imaging findings were compiled and analyzed in aggregate.Results
Among 15 patients with new clinical diagnoses of MM, 9 (60%) had FDG-avid bone lesions. In contrast, among the 10 patients with new clinical diagnoses of MGUS or SMM, none had FDG-avid bone lesions. Of the remaining 11 patients imaged for suspected recurrence or surveillance of previously treated MM, only 4 had FDG-avid bone lesions. Analysis of 20 FDG-avid bone lesions imaged on the same day with both PET/CT and PET/MRI revealed CT correlates for 15 lesions (75%) and MRI correlates for 14 lesions (70%). Notably, a single patient had 5 FDG-avid spinal lesions with CT correlates but without MRI correlates; however, no sagittal TSE T1WIs of the spine were acquired for this patient. Five of the 20 FDG-avid bone lesions were apparent on MRI but not CT (Fig 1). Using marrow biopsy and/or serum protein electrophoresis (SPEP) as a standard of reference, FDG-PET correctly differentiated metabolically active from inactive disease in 6 of 8 patients with previously treated MM. Active and inactive lesions were otherwise indistinguishable on MRI alone; both lesion types generally exhibited focal T2-hyperintensity and enhancement (Fig 2).Discussion
FDG-PET/MRI was successfully performed for both initial staging and subsequent treatment response assessment in patients with PCDs. FDG-PET correctly differentiated metabolically active from inactive disease in the majority of patients with previously treated MM. For cases in which sagittal TSE T1WIs of the spine were acquired, more lesions had MRI correlates than CT correlates. The addition of FDG-PET to whole-body MRI is useful for differentiating metabolically active and inactive disease, which can look identical on MRI alone. PET/MRI also provides substantial radiation dose reductions relative to PET/CT, especially in patients with malignancies such as MM that require frequent follow-up imaging studies.4 New PET tracers under development, such as those targeting VLA-4, may further expand the role of PET/MRI in PCDs by improving sensitivity for early or limited disease.5Conclusion
FDG-PET/MRI is feasible for both the initial staging and subsequent treatment response assessment of PCDs. To maximize the clinical utility of PET/MRI relative to PET/CT for the anatomic depiction of marrow-replacing lesions, sagittal TSE T1WIs images of the spine should be incorporated into standard protocols. Relative to MRI alone, FDG-PET/MRI is superior for differentiating metabolically active and inactive disease, especially in patients with suspected recurrence.Acknowledgements
No acknowledgement found.References
1. Hanrahan CJ, Christensen CR, Crim JR. Current Concepts in the Evaluation of Multiple Myeloma with MR Imaging and FDG PET/CT. Radiographics. 2010 Jan;30(1):127-42.2. Baur-Melnyk A, Buhmann S, Becker C, et al. Whole-body MRI versus whole-body MDCT for staging of multiple myeloma. American Journal of Roentgenology. 2008 Apr;190(4):1097-104.
3. Walker R, Jones-Jackson L, Rasmussen E, et al. Diagnostic Imaging of Multiple Myeloma-FDG PET and MRI Complementary for Tracking Short Vs. Long Term Tumor Response. Blood. 2004 Nov 16;104(11):758-8.
4. Schäfer JF, Gatidis S, Schmidt H, et al. Simultaneous whole-body PET/MR imaging in comparison to PET/CT in pediatric oncology: initial results. Radiology. 2014 May 31;273(1):220-31.
5. Soodgupta D, Zhou H, Beaino W, Lu L, Rettig M, Snee M, Skeath J, DiPersio JF, Akers WJ, Laforest R, Anderson CJ. Ex vivo and in vivo evaluation of overexpressed VLA-4 in multiple myeloma using LLP2A imaging agents. Journal of Nuclear Medicine. 2016 Apr 1;57(4):640-5.
Figures
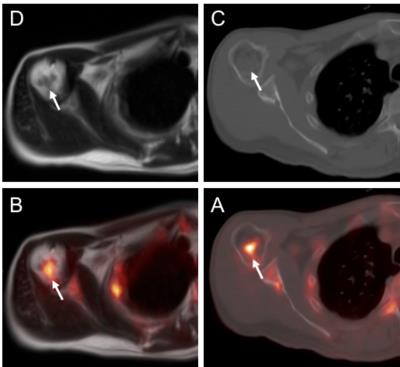
Improved
anatomic delineation of FDG-avid marrow-replacing lesions with MRI compared to CT.
A 53-year-old man with a new clinical diagnosis
of MM presented for initial staging and underwent FDG-PET/CT (B – transaxial CT
images, D – transaxial PET/CT fusion images) immediately followed by
FDG-PET/MRI (A – transaxial T2-weighted images, C – transaxial PET/MRI fusion
images). Among numerous FDG-avid lytic lesions, a focus in the proximal right
humerus with increased FDG uptake (arrows in C, D) had a clear T2-hypointense
correlate (arrow in A) but no definite CT correlate (arrow in D).
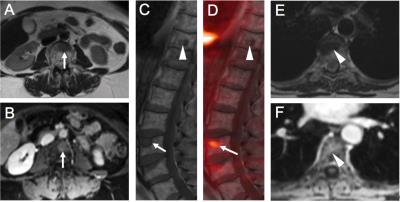
FDG-PET differentiates active and inactive myeloma, which can look similar on MRI. A 66-year-old woman with MM status-post stem cell transplantation (SCT) presented for restaging FDG-PET/MRI. Two T2-hypointense (A, E), enhancing (B, F) lesions were noted in the L3 (arrows) and T10 (arrowheads) vertebrae. Sagittal TSE T1WIs and FDG-PET fusion images (C, D) showed increased FDG uptake within the L3 lesion (arrow) but not the T10 lesion (arrowhead). The T10 lesion, which had demonstrated FDG-avidity prior to SCT (not shown), was deemed inactive myeloma. In contrast, the L3 lesion was interpreted as active myeloma given its FDG-avidity.