1290
A Hybrid ECG/Self-Navigation Technique1Medical Imaging, University Health Network, Toronto, ON, Canada, 2Medical Imaging, University of Toronto, Toronto, ON, Canada
Synopsis
In self-navigation, cardiac and respiratory information is extracted from the MR signal. ECG and conventional navigator echoes are not required. Conventional navigators disrupt the steady state and add delays. Thus, self-navigation provides a clear advantage. However, ECG is monitored independently of the MR acquisition. Therefore, eliminating the ECG needlessly throws away information. In this study, a hybrid ECG/self-navigated sequence is developed. ECG is used for cardiac triggering. Self-navigation is used for respiratory compensation, and to provide additional cardiac gating. In 10 healthy volunteers, the ECG/self-navigation sequence provided equivalent image quality and quantitative cardiac metrics as a reference breath-hold scan.
Introduction
In fully self-navigated techniques, information on the cardiac and respiratory cycles is extracted directly from the MR signal. Thus, ECG and navigator echoes are not required. Conventional navigator echoes disrupt the steady state and add delays to the pulse sequence. Thus, self-navigation provides a clear advantage in this regard. On the other hand, ECG is monitored independently of the MR acquisition. Moreover, it is typically performed in any event for patient safety monitoring. Therefore, other than convenience, eliminating the ECG needlessly throws away useful information.
Our objective is to develop a hybrid ECG/self-navigated sequence. ECG will be used for basic cardiac timing. Self-navigation will be used for two purposes: First, it will be used for respiratory compensation. Second, it will be used to provide information about the morphology of the heart. We speculate that this will provide additional (rather than simply redundant) information over and above the basic ECG timing. In this study, we will perform an initial assessment of this concept in healthy volunteers.
Theory
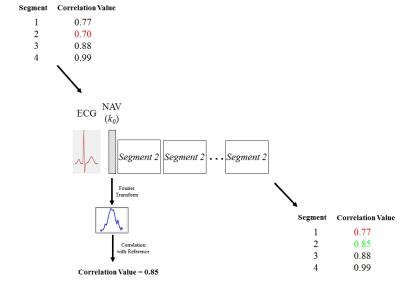
The ECG/self-navigated hybrid sequence is plotted in Figure 1. A regular ECG gating signal is acquired. Immediately after the R-wave is detected, a central k-space navigator line is acquired. Subsequently, a segment of k-space data is acquired (in cine mode).
The ECG provides the basic timing information for triggering the data acquisition. However, the decision as to whether to retain the data is governed by the navigator (Figure 2). Specifically, the navigator is correlated to an initial central k-space reference line (acquired at the beginning of the scan). If the correlation value is too low, the data is not retained. Furthermore, this same segment is reacquired on the next cardiac cycle. "Too low" in this context means that the correlation value is lower than the correlation value associated with all other segments. In this manner, the segment with the lowest correlation value is always being re-acquired. Note that with this approach, the navigation provides gating information on both cardiac and respiratory cycles.
Methods
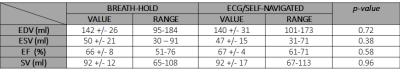
A total of ten healthy volunteers were imaged with ECG/self-navigation. Additionally, breath-hold scans were acquired as a reference. To evaluate the hybrid technique, two separate analyses were performed: First, end-diastolic volume (EDV), end-systolic volume (ESV), ejection fraction (EF), and stroke volume (SV) were quantified. Second, a visual assessment of image quality was performed independently by two cardiac radiologists. They were scored as follows: 0 = Non diagnostic, 1 = Poor quality, 2 = Fair quality, 3 = Good quality, 4 = Excellent quality. For both analyses, a t-test was performed to compare the ECG/self-navigated and breath hold scans. Statistical significance was set at the 95% confidence level.
Results
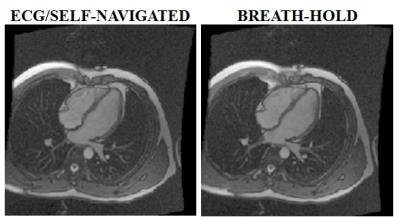
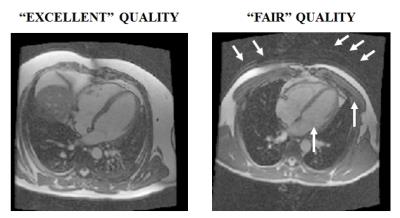
Figure 3 plots an example demonstrating the similar image quality that can be achieved between an ECG/self-navigated scans and the breath-hold reference. Both were rated as having "excellent" quality. Figure 4 is a plot illustrating the range of quality of ECG/self-navigated images. This example demonstrates images rated as "excellent" and "fair". The former image is largely artifact-free, whereas the latter exhibits some motion artifacts (arrows).
The overall image quality scores were 3.6+/- 0.6 for the breath-hold, and 2.8+/-0.7 for ECG/self-navigation. These scores were not statistically different -- although there was a trend toward higher scores with the breath-hold scans. In terms of absolute quality, 92% of the breath-hold scans and 70% of the navigator scans were rated as having good-to-excellent quality. No scans were rated as non-diagnostic.
Table 1 indicates no significant difference in any quantitative cardiac metric between ECG/self-navigation and reference breath-hold scans.
Discussion/Conclusions
The hybrid ECG/self-navigation technique clearly provides effective motion compensation. It achieved statistically equivalent quantitative cardiac metrics as well as image quality scores to the reference breath-hold technique. It also provided images with good to excellent quality in the most cases. On the other hand, although not statistically significant, a trend towards better image quality on the breath-hold scans was noted. However, note that the present study focused on the “best-case” scenario – healthy volunteers. In patients with limited breath-holding ability and higher heart rate variability, the performance of the conventional breath-hold approach may suffer more than the hybrid ECG/self-gating approach. Therefore, following the succeful demonstration in healthy volunteers, future work will focus on an assessment of the hybrid ECG/self-navigation technique in patients.Acknowledgements
This study was supported by GE HealthcareReferences
No reference found.Figures