1235
Two-dimensional susceptibility-weighted MRI at 1.5T: preliminary utility in the assessment of the fetal osseous spineXin Chen1, Guangbin Wang1, Tianyi Qian2, Wen Liu1, Xinhong Wei1, and Fei Gao1
1Shandong Medical Imaging Research Institute, Shandong University, Jinan, People's Republic of China, 2Siemens Healthcare, MR Collaborations NE Asia, Beijing, People's Republic of China
Synopsis
This study aimed to explore the utility of two-dimensional susceptibility-weighted imaging (2D-SWI) for assessing the fetal osseous spine. Whole-spine MRI was performed on fetuses, which included 2D-SWI and T2-weighted true fast imaging with steady-state precession (T2-TrueFISP) sequences. The image quality of the 2D-SWI was superior to the T2-TrueFISP, allowing for improved diagnostic accuracy in the diagnosis of spinal abnormities. 2D-SWI was valuable in elucidating the structures of the fetal osseous spine allowing for better assessment of spinal deformity, especially in the cervical segment of the spine.
Introduction
Spinal abnormity is a common type of congenital anomaly. The prognosis for an isolated hemivertebra is good. However, in the case of multiple vertebral anomalies such as spinal dysraphism, myelodysplasia, and segmental spinal dysgenesis, the treatment is more complex and the prognosis, poorer. An accurate prenatal diagnosis allows for a more accurate prognostic evaluation. MRI plays an increasingly important role in the assessment of fetal spinal abnormities without radiation exposure. It can be used prenatally to better delineate the involvement of neural elements associated with osseous spinal anomalies. However, with conventional fetal MRI, there is poor detail of the bone. This is a significant limitation of the use of MRI in assessing the bony structures of the fetal spine. Susceptibility-weighted imaging provides high contrast between bone and soft tissues. Bone, which produces low signal on MR imaging, is easily distinguished from the surrounding soft tissues. Thus the SWI sequences can be used to accurately diagnose prenatal spinal anomalies to allow for delivery planning and decisions regarding pregnancy interruption. Therefore, the purpose of our study was to explore the feasibility of two-dimensional susceptibility-weighted MRI in the assessment of the fetal osseous spine.
Materials and methods
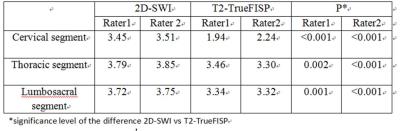
This prospective study was approved by our institutional review board. Written informed consent for participation was obtained from every pregnant woman. From November 2014 to May 2016, a total of 33 pregnant women having a median gestational age of 26 (range: 19–35) weeks with suspected fetal spinal abnormities were recruited. Fetal whole spinal MRI examinations were performed on a MAGNETOM Amira 1.5T MR Scanner (Siemens, Shenzhen Magnetic Resonance Ltd.,China) with body and spine array coils. Two-dimensional susceptibility-weighted imaging (2D- SWI) and T2-weighted true fast imaging with steady-state precession (T2-TrueFISP) images were obtained in axial, coronal, and sagittal planes. The scan parameters of the 2D-SWI were as follows: TR 85ms, TE 12.4ms, slices 8, slice thickness 3.0mm, slice gap 20%, FOV 300x 244mm2 , concatenations 2, resolution=0.6 x 0.6 x 3.0mm3, flip angle=15°; T2-TrueFISP: TR 560.9ms, TE 1.65ms, Slices 8, slice thickness 3.0mm, slice gap 20%, FOV 350x 286mm2, concatenations 1, resolution=1.3×1.3x 3.0 mm3, flip angle=76°. Two radiologists evaluated all images of the whole fetal spine in three segments (cervical, thoracic, and lumbosacral segments) independently. The image quality was evaluated on the basis of the outline depiction and the signal intensity of the osseous spine relative to that of the surrounding soft tissues using a 4-point grading scale: 1, poor (the osseous spine is not visible); 2, moderate (the osseous spine is poorly visible with a blurry outline); 3, good (the osseous spine is visible with a blurry outline); and 4, excellent (the osseous spine is clearly visible with a sharp outline). Inter-observer agreement for visualization scores from the two radiologists was calculated using a kappa statistic. The scores of the two sequences in the three segments were compared using a Wilcoxon's two-sample rank sum test.Results
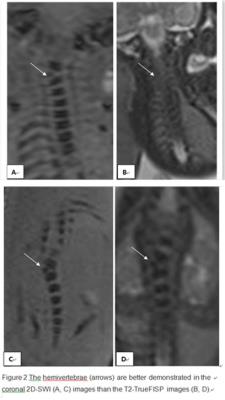
The inter-observer agreement was good both in the 2D-SWI (κ = 0.834) and T2-TrueFISP (κ = 0.774) images. The visualization scores of the 2D-SWI were higher than that of T2-TrueFISP in the three spinal segments, and the differences were significant. The detailed results are shown in Table 1. Of the 33 pregnant women, 11 women had detailed follow-up examinations. The clinical diagnoses of the 11 follow-up fetuses, were all in accordance with the 2D-SWI images taken prenatally, but only 4 were in accordance with T2-TrueFISP. 7 Of these, hemivertebrae were found in 4, butterfly vertebra in 2, spinal dysraphism in 3, and caudal regression syndrome in 2.Discussion
In previous studies, T2-TrueFISP and half-Fourier acquisition with single-shot turbo spin echo (HASTE) sequences were typically used for evaluating the fetal spine. However the images obtained by these methods cannot elucidate the detail of osseous structures. The results of this study demonstrate that 2D-SWI sequences provided excellent contrast between the osseous fetal spine and surrounding soft tissues compared with standard T2-TrueFISP, increasing the accuracy of the diagnosis of the spine deformity. In our study, 2D-SWI sequences provided the best contrast between the osseous fetal spine and the surrounding soft tissue in the cervical segment of the spine. Therefore, 2D-SWI could be useful in evaluating osseous fetal spine anomalies, particularly in the cervical segment of spine.Conclusion
2D-SWI was valuable in depicting the structures of the fetal osseous spine and assessing spinal deformities, particularly in the cervical segment of spine.