1220
A 64 Channel 3T Array Coil for Highly Accelerated Fetal Imaging at 22 Weeks of Pregnancy1A. A. Martinos Center for Biomedical Imaging, Massachusetts General Hospital, Charlestown, MA, United States, 2Department of Electrical Engineering and Computer Science, Massachusetts Institute of Technology, Cambridge, MA, United States, 3M+Visión Advanced Fellowship, Hospital Universitario de Fuenlabrada, Madrid, Spain, 4Boston Children’s Hospital, Boston, MA, United States, 5Harvard Medical School, Boston, MA, United States
Synopsis
MRI is an attractive tool for fetal imaging due to its unique ability to provide detailed anatomical and physiological data in an inherently safe manner. In practice, fetal MRI is limited by fetal motion, inherently poor SNR in the maternal abdomen, and widely varying body shapes. A 64 channel receive array designed to conform to a range of body shapes at 22 weeks of pregnancy was built and tested. Compared to standard product arrays, the coil provides 5% better SNR in the fetal brain region of an anthropomorphic phantom and allows increasing SENSE acceleration factor from R=4 to R=5.
Purpose
Fetal MRI is increasingly used in addition to ultrasound to evaluate possible fetal disorders. Indeed, MRI provides a higher soft tissue contrast in the fetus and reproductive organs. In order to minimize motion artifacts caused by fetal motion and to shorten acquisition times, high density arrays are needed. A standard fetal MRI protocol employs a spine array and a flexible torso array to reach approximately 34 channels. The major constraint of this implementation is the lack of anatomical fitting in the gravid abdomen and the possibility of highly accelerated acquisitions. In this work we designed a semi-adjustable, anatomically-shaped 64 channel array coil in order to maintain close fitting receive elements across different body shapes to maximize SNR in accelerated and unaccelerated imaging. The constructed coil addresses patient comfort concerns and can be deployed for robust daily use.Methods
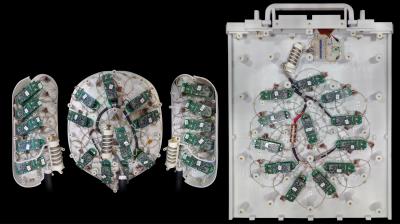
The coil was constructed on an anatomically shaped former consisting of four parts: a large posterior back panel with 24 elements that attaches to the direct connect table plug, an anterior belly panel with 20 elements, and two side wing panels with 10 elements each, adding up to 64-channels (Figs. 1,2). The coil panels are based on the segmented surface of a 22-weeks pregnant woman’s torso and printed in polycarbonate using a rapid prototyping 3D printer (Stratasys, Ltd., MN, USA). We used a projection of the geometrical decoupling arrangement [1] to accommodate the 3D circuitry of the loops. Geometric decoupling of nearest neighbor elements was optimized by pairwise manual adjustment of loop overlaps to minimize S12 measurements taken with a network analyzer. Next-nearest neighbor decoupling was achieved using preamplifier decoupling [1] performed by placing the inductance of the preamplifier input (as transformed by a 5.5cm coax cable and a series capacitor) in parallel with a loop capacitor to create a virtual open circuit. Data were acquired on a 3T Magnetom Skyra MRI system (Siemens Healthcare, Erlangen, Germany).
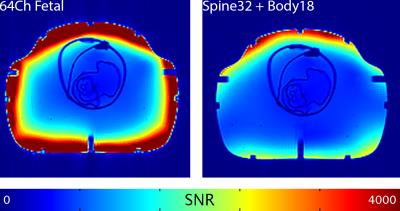
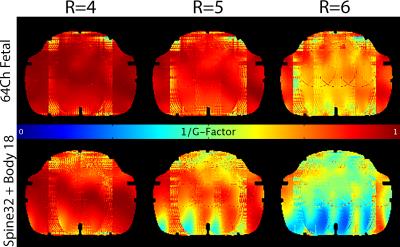
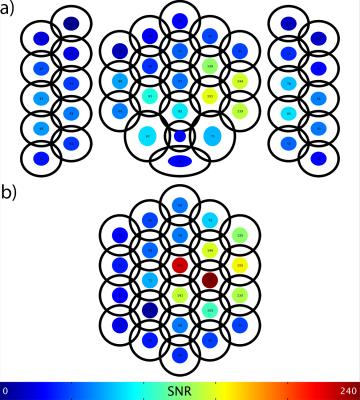
Preliminary testing was performed on a custom built anthropomorphic phantom based on the same segmented images as the coil itself. PD weighted images intersecting the fetal brain were acquired with a 2D GRE sequence (TR/TE/α =3500ms/7.1ms/45°, FoV=400mm, 7mm slice thickness, Matrix size: 192x192) using both the 64 channel fetal coil and the standard combination of 16 channels from a 32 channel spine array and all channels from an 18 channel flexible body array. Covariance weighted SNR and SENSE g-factor maps were computed using the resulting data. For the fetal coil, per-channel SNR maps were generated by dividing each of the 64 uncombined images by the standard deviation of a corresponding noise only image. The mean value of each single channel SNR map was computed for an ROI in the fetal brain region of the anthropomorphic phantom as a means of assessing the relative importance of each component in the array geometry.
Results
The 64 channel fetal coil achieved roughly 5% higher covariance weighted SNR inside the fetal brain region of the gravid abdominal phantom as compared to the standard array configuration (Fig. 3). Furthermore, it allowed an increase in SENSE acceleration factor from 4 to 5 in the RL direction and from 2 to 3 in the FH direction while maintaining acceptably low noise amplification levels (Fig. 4). Elements in the back panel contributed most to overall SNR in the fetal brain region, followed by the belly panel and side wings (Fig. 5). The QU/QL-ratio of a central loop in the belly panel was measured to be 318/35= 9.1.Discussion
The modest SNR improvement seen in unaccelerated imaging is likely attributed to the deep (nearly central) location of the fetal head where coil arrays with more than 16 elements already approach the ultimate SNR available [2]. Nonetheless, there is an improvement in acceleration capability likely due to the higher number of channels (64 vs. 34), achieving the SNR with array elements with higher spatial frequency content sensitivity profiles.
Because the same body models were used as references in the design of the coil and the phantom it was tested on, the two objects fit together very well. As this close fit is one of the noted advantages of the coil, further testing on human volunteers is needed to fully assess its relative performance.
Conclusion
A 64 channel array channel for fetal imaging at 22 weeks was constructed and compared to a standard 34 channel abdomen array configuration. The fetal coil achieves 5% better SNR in the brain region of a test phantom and allows increasing SENSE acceleration factor from R=4 to R=5.Acknowledgements
Support comes from NIH NICHD U01HD087211 and NIH NIBIB R01EB017337.References
[1] Roemer PB et al, MRM 16, 1990.
[2] Wiesinger F et al, MRM 52, 2004.
Figures