1185
Ventilation heterogeneity of pediatric cystic fibrosis accessed via lung clearance index and hyperpolarized 129Xe MRI1Center for Pulmonary Imaging Research, Division of Pulmonary Medicine and Department of Radiology, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States, 2Division of Pulmonary Medicine, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, United States
Synopsis
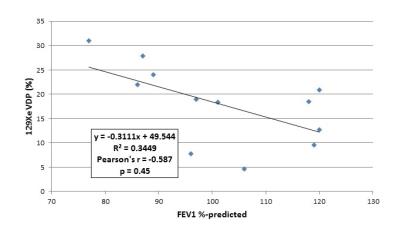
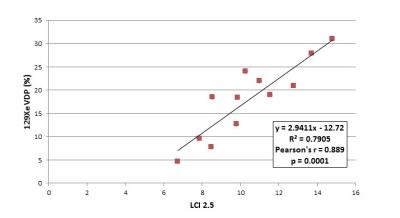
Quantitative hyperpolarized 129Xe ventilation MRI was compared to FEV1, the spriometric gold standard for assessing lung function, and lung clearance index (LCI), an emerging pulmonary function test to assess global ventilation heterogeneity, in 12 pediatric cystic fibrosis subjects. A range of severity and spatial distributions of 129Xe ventilation deficits were observed, with a 129Xe ventilation defect percentage (VDP) of 18.0% ± 8.1%. VDP did not correlate with FEV1 (p=0.45) but correlated very strongly with LCI (p=0.0001), suggesting that the spatial distribution of defects in the 129Xe images represents obstructed areas of the lung that give rise to elevated LCI.
Purpose
The clinical gold standard for assessing lung disease severity is the forced expiratory capacity in one second (FEV1) from spirometry, yet this metric has well-recognized shortcomings, including a complete lack of regional information and low sensitivity to early disease. This insensitivity is especially problematic in pediatric-onset disorders, such as cystic fibrosis (CF), in which lung disease progression begins shortly after birth but were functional deficit—as measured by spirometry—often cannot be observed until patients are in their teens. As a means of providing both spatial information and high sensitivity to functional impairment, hyperpolarized 129Xe gas is a safe and effective inhaled imaging agent for the pulmonary imaging of adults1, 2 and children3. The purpose of this study was to compare regional ventilation deficits quantified via 129Xe MRI to FEV1 and to ventilation heterogeneity from a multiple-breath N2 washout technique (lung clearance index, LCI) that has emerged as a research standard in the cystic-fibrosis and other pulmonary-research communities.Methods
Hyperpolarized 129Xe MRI was performed in 12 pediatric CF subjects (3 males and 9 females; age range 8-16 years old; mean ± SD FEV1 %-predicted 101.3% ± 15.2%) using Xe gas prepared by either a commercial (Polarean Inc, Durham, NC) or homebuilt polarizer4. After 1H localization scans and a small 129Xe in vivo flip-angle calibration dose, 129Xe ventilation images (FA = 9-14°; TR/TE = 8 ms/4 ms; matrix = 52-96 x 96-144; voxel = 3 x 3 x 15 mm3; 9-14 slices based on subject size) were acquired on a Philips 3T Achieva MRI scanner with a homebuilt saddle coil5 during a single breath-hold to up to 16 seconds. Xe gas was dosed at 1/6th predicted total lung capacity based on subject sex and height6. Subject heart-rate and blood oxygenation (SpO2) monitored throughout the protocol. Ventilation deficits were identified using semi-automated image segmentation and processing in R, and global ventilation defect percentage (VDP) was determined using a 60% mean whole-lung 129Xe signal threshold. LCI was performed by trained clinical staff using multiple breath wash-out technique with N2. VDP was compared to LCI2.5 (lung clearance index to achieve 2.5% of the starting N2 concentration) and FEV1 from clinical records using Pearson correlations.Results
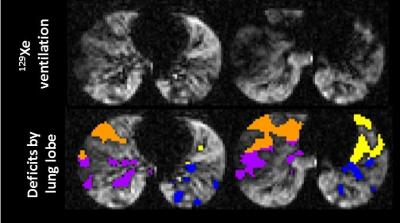
All subjects tolerated the 129Xe MRI protocol and no serious adverse events were reported. Ventilation deficits were visually apparent in all subjects with a wide range of heterogeneity and lobar distribution (Figure 1); the mean ± SD 129Xe VDP was 18.0% ± 8.1%, with a range of 4.6-27.9%. Ventilation deficits were even apparent in subjects with high FEV1; however, there was wide range of VDPs observed in subjects with similar FEV1s (Figure 2). VDP was not significantly correlated with FEV1, with a Pearson’s coefficient r = -0.587 and p = 0.45. 129Xe VDP was significantly associated with LCI2.5, with Pearson’s r = 0.889 and p = 0.0001; this is detailed in Figure 3.Discussion
Ventilation defects in early CF lung disease are readily apparent, even in subjects without clinical manifestations of lung disease (FEV1> 90%), suggesting that the imaging is detecting early pre-clinical obstruction, as also evidenced by LCI. The strong correlation between 129Xe VDP and LCI2.5 suggests that global ventilation heterogeneity assessed by LCI captures some aspects of regional lung obstruction and ventilation deficits seen clearly in the 129Xe ventilation images. Furthermore, 129Xe MRI may provide a sensitive, novel imaging-based biomarker for the clinical trials of new therapies in diseases where patient numbers are low (e.g., rare CF gene mutations and rare lung diseases), or even in individual patients.Conclusion
129Xe VDP correlated very strongly with LCI, suggesting that both metrics assess ventilation heterogeneity; however, 129Xe MRI provides additional regional, pathological information currently unavailable from any global assessment of lung function. Furthermore, 129Xe ventilation images can be co-registered with 1H MR images (e.g., ultrashort echo time, UTE) to reveal regional lung structure-function relationships. The spatial information from 129Xe MRI can be used to plan bronchoscopies or to assess the efficacy of new CF therapeutics, even in single-patient trials.Acknowledgements
No acknowledgement found.References
1. Driehuys, B., S. Martinez-Jimenez, Z.I. Cleveland, et al., Chronic Obstructive Pulmonary Disease: Safety and Tolerability of Hyperpolarized Xe-129 MR Imaging in Healthy Volunteers and Patients. Radiology, 2012. 262(1): 279-289.
2. Shukla, Y., A. Wheatley, M. Kirby, et al., Hyperpolarized 129Xe magnetic resonance imaging: tolerability in healthy volunteers and subjects with pulmonary disease. Acad Radiol, 2012. 19(8): 941-51.
3. Walkup, L.L., R.P. Thomen, T. Akinyi, et al., Feasibility, Tolerability, and Safety of Pediatric Hyperpolarized 129Xe Magnetic Resonance Imaging in Healthy Volunteers and Subjects with Cystic Fibrosis. Pediatric Radiology, 2016. 46(12): 1651-1662.
4. Walkup, L.L., R.P. Thomen, N.S. Higano, et al., Initial experience performing hyperpolarized 129Xe MRI in young, pediatric subjects using a homebuilt Xe polarizer, in Experimental Nuclear Magnetic Resonance Conference. 2016: Pittsburgh, PA.
5. Loew, W., R. Thomen, R. Pratt, et al., A Volume Saddle Coil for Hyperpolarized 129Xe Lung Imaging. Proc. Intl. Soc. Mag. Reson. Med, 2015. 23: 1507.
6. Stocks, J. and P.H. Quanjer, Reference values for residual volume, functional residual capacity and total lung capacity. ATS Workshop on Lung Volume Measurements. Official Statement of The European Respiratory Society. Eur Respir J, 1995. 8(3): 492-506.
Figures