1164
Management of complex regional pain syndrome (CRPS) with [18F]FTC-146 PET/MRI1Department of Radiology, Stanford university, Palo Alto, CA, United States, 2The Intervention Centre, Oslo University Hospital, Oslo, Norway, 3The Norwegian Medical Cyclotron Centre, Oslo, Norway, 4Department of Anesthesiology, Stanford university, Palo Alto, CA, United States, 5Department of Surgery, Stanford university, Palo Alto, CA, United States, 6Department of BioMolecular Sciences, The University of Mississippi
Synopsis
Complex regional pain syndrome (CRPS) is a debilitating chronic pain condition affecting millions of patients worldwide. However, no specific diagnosis is currently available to accurately detect the pain generators in CRPS, and thus successful pain management for CRPS is very challenging. In this abstract, we propose a PET/MRI approach with a novel pain-specific PET tracer for identifying pain generators in CRPS. Our early experience with the proposed PET/MRI approach demonstrates that the image findings could alter the pain management for CRPS patients to achieve better pain-relief outcome.
Purpose
To assess the clinical impact of our proposed [18F] FTC-146 PET/MRI method on pain management for complex regional pain symptom (CRPS) patients.Introduction
Complex regional pain syndrome (CRPS) is a severe chronic pain condition affecting millions worldwide with an incidence of 50,000 new cases/year in the U.S. alone1. Unfortunately, there is no specific diagnostic test to identify the pain generators in CRPS, leading to poor pain management planning. Recently, an [18F]FDG PET/MRI approach demonstrated that the hotspots of [18F]FDG uptake indicating locally increased metabolism could be an effective marker for pain generators2. However, not all increased [18F]FDG uptake can be attributed to sites of pain or inflammation, and thus the findings of [18F]FDG PET/MRI are sometimes non-specific to pain. In this abstract, we propose a more pain-specific PET/MRI approach for CRPS, adopting a highly selective sigma-1 receptor (S1R) PET radioligand, [18F]FTC-146. [18F]FTC-146 provides detection of nociceptive and inflammatory physiologic processes given S1R’s strong association for pro-nociceptive processes3,4. We studied the impact of our proposed approach on pain diagnosis management for CRPS patients.Methods
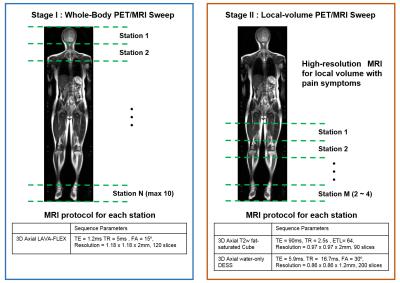
8 patients suffering from CRPS were referred directly from specialists in pain medicine. The patients were imaged with a 3T GE SIGNA PET/MRI system. Radiosynthesis of clinical grade FTC-146 was performed and administered in human subjects under an IRB and FDA-approved exploratory Investigational New Drug trial (NCT02753101). All patients underwent PET/MR imaging immediately after a single 10 mCi intravenous injection of [18F]FTC-146. The imaging procedure was composed of two stages. In the first stage, patients were scanned from the head through the feet. 8 to 10 imaging stations were prescribed to scan each body segment as shown in Figure 1. In each station, a 3D axial LAVA-FLEX MRI scan was acquired simultaneously with the PET scan. In the second stage, 2 to 4 imaging stations were prescribed to scan local volume covering the areas of pain symptom with a high-resolution 3D axial DESS scan and a 2D axial T2-weighted FSE scan.
We analyzed the uptake pattern of [18F]FTC-146 in PET scans and anatomic abnormalities in MR scans. We summarized the new findings from our PET/MRI studies, and discussed the findings with the referring pain specialists. Alterations in the pain management plan based on our PET/MRI findings were recorded and the patients were followed. In a subset of cases, new treatments were applied and standard pain measures (pain numeric rating scale and clinical exam) were recorded to assess the impact of the PET/MRI approach on the outcomes and pain-level of the patient.
Results and Discussion
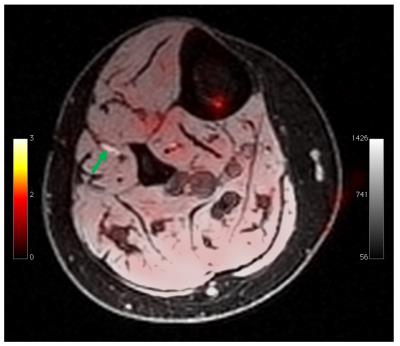
The PET/MRI overlaid image in Figure 2 demonstrates the specificity of [18F]FTC-146 to pain. The bright lesion pointed by green arrow is a neuroma, which may or may not cause pain. Physical examination confirmed that the neuroma was non-painful, and, correspondingly, no significant [18F]FTC-146 uptake was observed in the neuroma.
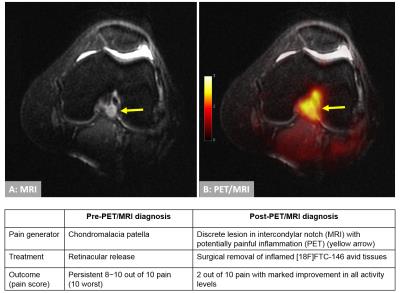
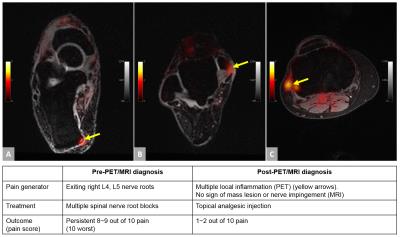
Figure 3 demonstrates one successful treatment of a CRPS patient based on our PET-MRI findings. This patient had severe, persistent knee pain despite 2 previous unsuccessful surgeries that were based on clinical exam and conventional MRI. [18F]FTC-146 PET/MRI showed a high, focal [18F]FTC-146 uptake of a lesion on PET which co-localized to an abnormal high-signal lesion in the intercondylar notch of the symptomatic knee on the MR images. Arthroscopic surgery was performed to remove the [18F]FTC-146-avid lesion, which successfully relieved the knee pain. Figure 4 summarizes another successful pain-relief case of a CRPS patient with chronic hip and foot pain. The patient previously had unsuccessful history of multiple spinal nerve blocks. We found high [18F]FTC-146 uptake on multiple focal spots in the knee and foot, and MRI showed no mass lesion or possible nerve impingement (that would normally require surgery). Local anesthetic and steroid injection on the areas of high [18F]FTC-146 uptake was followed, and patient reported a significant improvement in pain score.
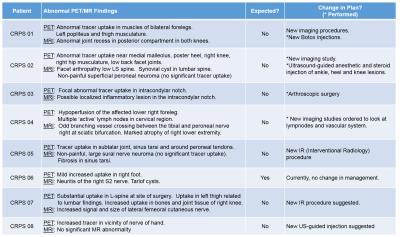
Figure 5 summarizes findings on the 8 CRPS patients studied thus far with our PET/MRI method. Seven out of 8 patients showed unexpected findings on PET/MRI, which lead to a change in the patients’ pain management plans. Not all of the changed plans have been executed yet, and we will continue to follow the patients to further evaluate our image findings.
Conclusion
In this abstract, we introduced a whole-body PET/MRI approach with a novel pain-specific PET tracer, [18F]FTC-146, to identify pain generators in CRPS. Our early clinical experience suggests that the new image findings from the proposed PET/MRI method could alter the pain management for CRPS patients to achieve improved outcomes and more effective treatments for pain.Acknowledgements
NIH R01 AR0063643, NIH P41 EB015891, NIH R01 DA023205, NIH P20 GM104932, GE Healthcare.References
1. A.T. Borchers, and M.E. Gershwin, Complex regional pain syndrome: a comprehensive and critical review. Autoimmun Rev, 13(3): p. 242-65, 2014.
2. Yoon D, Behera D, Holley D, Gallant P, Ith MAM, Carroll I, Smuck M, Hargreaves BA, Biswal S. [18F]FDG PET/MRI of Patients With Chronic Pain Alters Management: Early Experience. Proc. Intl. Soc. Mag. Res. Med., p. 0883, 2016.
3. T. Maurice. and T.P. Su, The pharmacology of sigma-1 receptors. Pharmacol Ther, 124(2): p. 195-206, 2009.
4. M.L. James et al., Evaluation of sigma-1 Receptor Radioligand 18F-FTC-146 in Rats and Squirrel Monkeys Using PET. J Nucl Med, 55(1): p. 147-53, 2014.
Figures