1149
Dynamic knee imaging using 4D self-gated MRI with compressed sensing reconstruction1Department of Radiology, Academic Medical Center, Amsterdam, Netherlands, 2Biomedical NMR, Department of Biomedical Engineering, Eindhoven University of Technology, Eindhoven, Netherlands, 3Orthopaedic Research Lab, Radboud UMC, Nijmegen, Netherlands, 4Biomedical Engineering and Physics, Academic Medical Center, Amsterdam, Netherlands, 5Department of Radiology, University Medical Center Utrecht, Utrecht, Netherlands
Synopsis
Knee abnormalities and pain are sometimes elucidated during motion, therefore the ability to obtain 4D images of the moving knee could add diagnostic value to the conventional static MRI scans. In this work we present a method to obtain 4D imaging of the human knee during motion, without the use of an external gating system.
Purpose
To develop a method to obtain 4D imaging of the human knee during motion, without the use of an external gating system.Introduction
Anatomical (static) MRI is the most commonly used imaging technique for evaluation and assessment of the knee joint, but does not provide dynamic information and does not allow studying the interaction of the different tissues during motion. Since knee pain is often only experienced during dynamic tasks, the ability of obtaining 4D images of the knee during motion could improve diagnosis and provide a deeper understanding of the knee joint. In this work we present a novel approach for dynamic, high-resolution 3D imaging of the freely moving knee without a need for external triggering. The protocol is based on a self-gated 4D stack-of-stars radial sequence with compressed sensing reconstruction. To evaluate the effects of non-uniform motion and poor coordination skills on the quality of the reconstructed images, we performed a comparison between fully free movement and movement instructed by a visual cue.Methods
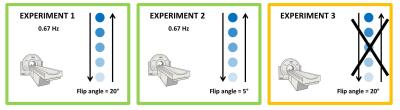
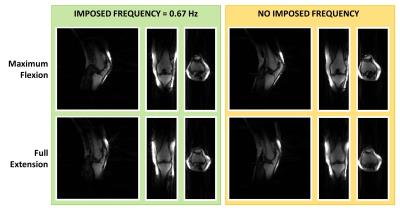
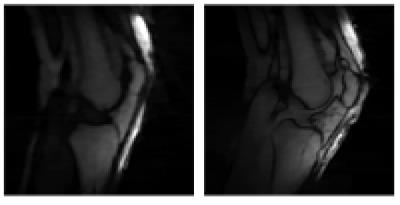
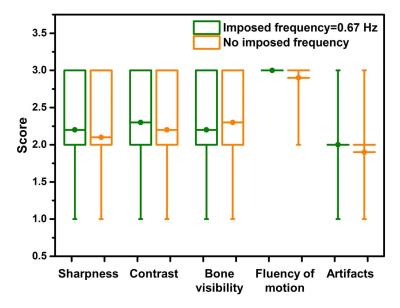
The dominant knee of 5 female volunteers (mean age=27±1 kg mean weight=61±6 kg) with no history of knee injury or pain was scanned. The subjects were placed supine on the scanner table, with a triangular-shaped support underneath their knees, and they were asked to perform a knee flexion/extension task 3 times. The 3 experiments performed with each subjects are illustrated in Figure 1. The dynamic scans were obtained using a golden angle stack-of-stars radial gradient-spoiled gradient-echo sequence implemented on a 3T Philips Ingenia scanner (Philips, Best, The Netherlands). Sequence parameters were: matrix size = 160x160x47, voxel size=1.5x1.5x3 mm3, FOV=240x240x141 mm3, TR=3.9 ms, TE=1.3 ms. A total of 1410 spokes was acquired for each stack, with a tiny golden angle increment of ~20.89°1, using a zy-ordering approach. The acquisition was done continuously during 5 minutes and 20 seconds of knee flexion/extension. All acquisitions were performed using a custom built 15 ch flexible coil array (MR Coils BV, The Netherlands) (Figure 2a) in combination with the 8 elements embedded in the scanner table. Image reconstruction was performed in Matlab. The synchronization signal required for self-gating was derived from the center of k-space of the 3 middle slices, after inverse Fourier transformation in the z-direction and array compression. The trigger extraction was based on Principal Component Analysis (PCA), to determine the most common signal variations from the 10 coil elements. The Principal Component representing knee motion was then selected as the one with the highest peak in the selected frequency band (Figure 2). The knee motion was subsequently binned in 20 motion states2. We used the BART toolbox3 to perform a parallel-imaging CS reconstruction with a spatial and temporal total-variation l1-regularization (r=0.01, 100 iterations). Sensitivity maps were estimated for each frame individually using the ESPIRiT method4. The movies obtained with and without instructions were compared by two MDs with experience in MRI in terms of sharpness, contrast, bone visibility, fluency of motion, and presence of artifacts.Results
Volunteers were able to perform the motion task very consistently when instructed via a visual cue (narrow frequency peak, Figure 2d). On the other hand, the lack of precise instructions led to a shift of the center motion frequency, together with a broadening of the peak. However, with PCA for self-gating, the frequency representing both instructed and uninstructed motion could be identified correctly and resulting images only showed minor motion blurring (Figure 3 and 4). Additionally, using a low flip angle, we could obtain high signal from collagen-rich structures such as Posterior Cruciate Ligament, Anterior Cruciate Ligament and cartilage. No significant difference in image-quality scoring was reported for the movies obtained with and without instructions (Figure 5).Discussion
Kaiser et al.5 have developed a 4D MRI imaging technique to study tibiofemoral kinematic in healthy subjects which makes use of a kooshball encoding scheme and constant monitoring of knee flexion angle, which is retrospectively used for sorting radial spokes into several frames. Using our method, we were able to obtain 4D high resolution of the knee without the need for external hardware for gating. PCA showed to be a robust method to extract self-gating signal even for uninstructed motion. Therefore the technique is potentially suitable also for patients that due to pain may find difficult to exactly comply with instructions. Although contrast manipulation remains challenging in dynamic imaging due to time constrains, we have shown the possibility to enhance either the bones or soft tissues, like ligaments and cartilage. Further work will focus on accurate extraction of kinematics parameters from the obtained 4D data.Acknowledgements
No acknowledgement found.References
1 S. Wundrak, J. Paul, J. Ulrici, E. Hell and V. Rasche, "A Small Surrogate for the Golden Angle in Time-Resolved Radial MRI Based on Generalized Fibonacci Sequences," in IEEE Transactions on Medical Imaging, vol. 34, no. 6, pp. 1262-1269, June 2015. doi: 10.1109/TMI.2014.2382572
2 Feng, L., Axel, L., Chandarana, H., Block, K. T., Sodickson, D. K. and Otazo, R. (2016), XD-GRASP: Golden-angle radial MRI with reconstruction of extra motion-state dimensions using compressed sensing. Magn. Reson. Med., 75: 775–788. doi:10.1002/mrm.25665
3BART: version 0.3.01 (2016) DOI: 10.5281/zenodo.50726
4 Uecker, M., Lai, P., Murphy, M. J., Virtue, P., Elad, M., Pauly, J. M., Vasanawala, S. S. and Lustig, M. (2014), ESPIRiT—an eigenvalue approach to autocalibrating parallel MRI: Where SENSE meets GRAPPA. Magn. Reson. Med., 71: 990–1001. doi:10.1002/mrm.24751
5 Kaiser, J., Bradford, R., Johnson, K., Wieben, O. and Thelen, D. G. (2013), Measurement of tibiofemoral kinematics using highly accelerated 3D radial sampling. Magn Reson Med, 69: 1310–1316. doi:10.1002/mrm.24362
Figures