1076
Inflammatory activity of Crohn's disease: Evaluation by MR T2*mapping without intravenous enhancement1Department of Radiology, The First Affiliated Hospital of Sun Yat-Sen University,Guangzhou, China, Guangzhou, People's Republic of China, 2Department of Biomedical Engineering, Cancer Biology and Radiology, Wake Forest School of Medicine, 3Department of Radiology, Hospital of Stomatology, Guanghua School of Stomatology, Sun Yat-Sen University, Guangdong Provincial Key Laboratory of Stomatology, 4Department of Radiology, Conde de S. Januario Central Hospital, Macau
Synopsis
Crohn's disease (CD) is a chronic relapsing inflammatory bowel disease leading to structurally irreversible bowel damage. The incidence of CD had been increasing in the past century epidemiologically . Accurate evaluation of CD activity is crucial for new therapeutic goals of mucosal healing, preventing bowel damage, limiting disability, and improving quality of life . Although colonoscopy remains the gold standard for assessing CD activity, it is invasive, limited to assessment of the small bowel, and not suitable for continuing monitoring of CD activity . Thus, seeking for alternative noninvasive and accurate approaches to assess CD activity is necessary.
Purpose
Crohn's disease (CD), a chronic relapsing inflammatory bowel disease, often results in structurally irreversible bowel damage. Accurate evaluation of CD activity is crucial for new therapeutic goals of mucosal healing, preventing bowel damage, limiting disability, and improving quality of life.Magnetic resonance enterography (MRE) is a technique that involves the use of MR imaging (MRI) to assess especially the small bowel.MR T2* mapping has the potential for reflecting tiny change on biochemical components of the counterpart without contrast medium injection. It remains unclear whether T2* mapping could differentiate grades of inflammation activity in Crohn’s disease (CD). In this study, we aim to assess the efficacy of T2* mapping for evaluating CD activity compared to conventional magnetic resonance enterography (MRE).
Method
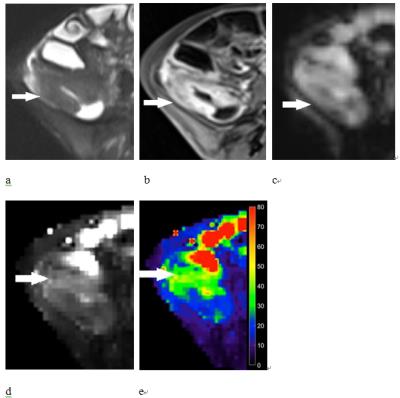
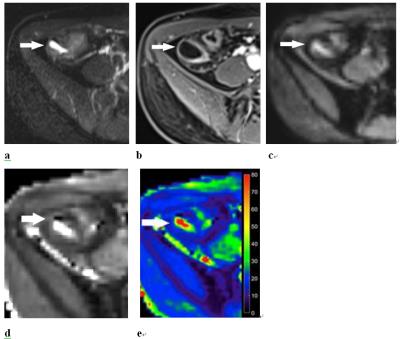
We performed an observational study conducted from August 2014 to December 2015of a single-center cohort which inclusive criteria were established CD diagnosis by conventional clinical, endoscopic and histologic criteria for all patients. 98 adults diagnosed of CD underwent MRE and T2*-weighted MR imaging. The disease activity was scored by Magnetic Resonance Index of Activity (MaRIA) as inactive (<7), mild (≥7 and <11) or moderate-severe (≥11). T2* values of thickened bowel wall were measured on T2* mapping, compared to conventional MRE and correlated with MaRIA.Result
All of the bowel segments in the enrolled 98 patients presented acceptable image quality on MR were evaluated. The difference in T2* values of 160 bowel segments among inactive (26), mild (23) and moderate-severe (111) CD was significant (all P<.001). T2* value correlated significantly with MaRIA (r=0.743) better than mural thickness (r=0.611), relative contrast enhancement (r=0.473) and ulceration (r=0.309). T2* value was accurate with good inter-observer agreement for distinguishing inactive from active CD (AUC=0.877) and differentiating inactive-mild from moderate-severe CD (AUC=0.848). The threshold T2* value of 15.94 ms was 93.3% sensitive and 72% specific for distinguishing active from inactive CD whereas T2* value of 20.00 ms was 74.5% sensitive and 84.0% specific for differentiating inactive-mild from moderate-severe CD.Discussion
Assessing CD activity is extremely important for treatment plan. Researchers have been searching for a brief, noninvasive and accurate method to evaluate inflammatory activity of CD without complicated calculation. MaRIA was with cockamamie calculations and was not convenient for routine clinical application. Despite above limitation, it can be considered as the most validated mean for assessing inflammation by MRI in CD. The efficacy of conventional MRE has been widely introduced in CD but little attention has been paid to the interest of T2*WI. According to our knowledge, our study is the first observational study to assess the accuracy of T2*WI in evaluating bowel inflammation in CD by comparing findings of T2* mapping and conventional MRE.Conclusion
T2* values correlated well with CD activity and T2* mapping is a promising novel imaging tool for evaluating activity of CD and monitoring therapeutic effect.Acknowledgements
The first draft of the article was written by Si-yun Huang. All authors reviewed and approved the final manuscript. No writing assistance was used.References
1. Peyrin-Biroulet L, Cieza A, Sandborn WJ, et al. Development of the first disability index for inflammatory bowel disease based on the international classification of functioning, disability and health. Gut 2012; 61:241-247.
2. Annese V, Daperno M, Rutter MD, et al. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis 2013; 7:982-1018.
3. Takenaka K, Ohtsuka K, Kitazume Y, et al. Comparison of magnetic resonance and balloon enteroscopic examination of the small intestine in patients with Crohn's disease. Gastroenterology 2014; 147:334-342.
4. Makanyanga JC, Taylor SA. Current and future role of MR enterography in the management of Crohn disease. AJR Am J Roentgenol 2013; 201:56-64.
5. Benitez JM, Meuwis MA, Reenaers C, Van Kemseke C, Meunier P, Louis E. Role of endoscopy, cross-sectional imaging and biomarkers in Crohn's disease monitoring. Gut 2013; 62:1806-1816.
6. Ordas I, Rimola J, Rodriguez S, et al. Accuracy of magnetic resonance enterography in assessing response to therapy and mucosal healing in patients with Crohn's disease. Gastroenterology 2014; 146:374-382.
7. Panes J, Bouhnik Y, Reinisch W, et al. Imaging techniques for assessment of inflammatory bowel disease: joint ECCO and ESGAR evidence-based consensus guidelines. J Crohns Colitis 2013; 7:556-585.
8. Rimola J, Ordás I, Rodriguez S, et al. Magnetic resonance imaging for evaluation of Crohn's disease. Inflamm Bowel Dis 2011; 17:1759-1768.
9. Yu S, Qiu J, Zhang J, Pan L, Xing S, Zhang L. Detection of intratumoral susceptibility signals using T2*-weighted gradient echo MRI in patients with clear cell renal cell carcinoma. PLoS One 2013; 8:e79597.
10. Mokhtar GM, Ibrahim WE, Elbarbary NS, Matter RM, Ibrahim AS, Sayed SM. Pancreatic functions in adolescents with beta thalassemia major could predict cardiac and hepatic iron loading: relation to T2-star (T2*) magnetic resonance imaging. J Investig Med 2016; 64:771-781.
11. Ellingson AM, Nagel TM, Polly DW, Ellermann J, Nuckley DJ. Quantitative T2* (T2 star) relaxation times predict site specific proteoglycan content and residual mechanics of the intervertebral disc throughout degeneration. J Orthop Res 2014; 32:1083-1089.
12. Macarini L, Stoppino LP, Centola A, et al. Assessment of activity of Crohn's disease of the ileum and large bowel: proposal for a new multiparameter MR enterography score. Radiol Med 2013; 118:181-195.
13. Seo N, Park SH, Kim KJ, et al. MR Enterography for the Evaluation of Small-Bowel Inflammation in Crohn Disease by Using Diffusion-weighted Imaging without Intravenous Contrast Material: A Prospective Noninferiority Study. Radiology 2016; 278:762-772.
Figures