1014
Effects of 5 alpha-Reductase Inhibitors on Detection of Prostate Cancer on MRI1Radiology, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States, 2Urology, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States
Synopsis
5 alpha reductase inhibitors have shown promise in increasing the detection of prostate cancer in prior ultrasound studies. No studies have been performed looking at the effect of 5 alpha reductase inhibitors on increasing the conspicuity of prostate cancer in MRI. The purpose of this study was to determine if treatment with a 5 alpha reductace inhibitor could increase sensitivity for the detection of prostate cancer in the background setting of benign prostatic hypertrophy.
Purpose
The purpose is to determine if 5 alpha-reductase inhibitors (5ARI) increase the conspicuity of prostate cancer on MRI, especially in the background of benign prostatic hypertrophy nodules.Methods
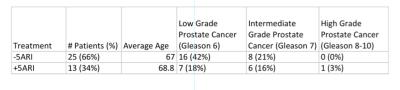
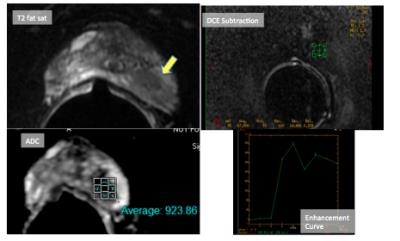
IRB approved retrospective study of men who underwent prostate MRI for elevated prostate specific antigen or abnormal digital rectal exam was performed. 38 men with biopsy proven prostate cancer by transrectal ultrasound (TRUS) guided biopsy were divided into a group of 13 men on a 5ARI for at least three months and 25 men not on a 5ARI. Two radiologists, who were blinded to the use of 5ARI, reviewed the prostate MRIs. The ADC value, the maximum enhancement over baseline unenhanced tissue, and the enhancement kinetic curves of the prostate cancer and a representative benign prostatic hypertrophy nodule were measured. Statistical analysis was performed using MedCalc for Widows, version 16.8.4.Results
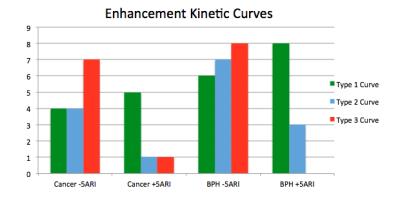
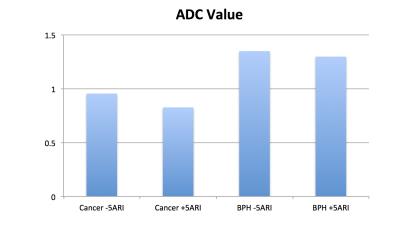
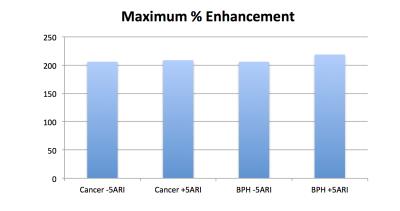
Average age of men included in the study was 67.6. Due to technical error, there was a failure of Gd contrast in two caes, but ADC data was still available. Cancer was not detected on 15 (39%) and BPH nodules were not identified on 3 MRIs (8%). There were less aggressive enhancement kinetic curves in patients on 5ARI in both the cancer and BPH nodules, which approached statistically significant in cancer lesions (p=0.0655) and was statistically significant in BPH nodules (p=0.0085). There was a slight decrease in ADC values in patients on 5ARI in both groups that was not statistically significant (p= 0.0991 and p=0.6975, respectively). There was minimal increased enhancement over baseline that was greater in the BPH nodules compared to the prostate cancer, but this was not statistically significant (p=0.9347 and p=0.6616, respectively).Discussion
Previous studies demonstrated that 5ARI’s decreased blood flow to benign prostatic tissue 1,2 on color Doppler US. To our knowledge there have been no studies performed on imaging characteristics of the prostate in response to 5ARI treatment other than volume. Pretreating with a 5ARI did not help localize prostate cancer for TRUS 3, but again no literature was identified using a 5ARI to help detect prostate cancer on MRI. There is an ongoing study looking at the effect of a 5ARI on prostate cancer volume on MRI in men undergoing active surveillance but the results have not been published 4. A difference between our MRI study and the US studies was that patients were treated with 5ARI as short-term pretreatment before ultrasound examination (1-3 weeks), whereas our patients were on long-term 5 ARI treatment for obstructive lower urinary tract symptoms for a minimum of 3 months. To our knowledge, there is no data available on the effect of a 5ARI on prostatic blood flow outside of the short-term US studies previously described. A 5ARI may be useful in suppressing the blood flow and enhancement of benign prostatic tissue and increase the conspicuity of cancerous lesions on MRI. The results of our preliminary study demonstrate that there is a downward shift in the aggressiveness of enhancement kinetic curves in both prostate cancer and BPH nodules. That the cancerous lesions only approached statistical significance could be related to our small data set. The simultaneous decrease in aggressiveness of enhancement kinetics did not make cancer more conspicuous. Treatment with 5ARI did not have a significant effect on enhancement or ADC values in either group. Many of the biopsy samples contained only 1% cancer and likely explains to the high number of cancers undetected by MRI.Conclusion
There is a trend towards less aggressive enhancement kinetics in both cancer and BPH nodules with 5ARI treatment. Although in this study the detection of prostate cancer on MRI was not increased, the effects of 5ARI on prostate MRI imaging characteristics deserve further evaluation. Given the long lead time of 5ARI treatment in this study (at least 3 months), compared to prior studies that determined an optimal pre-treatment time of 2-3 weeks to decrease blood flow in benign prostate tissue on US, we may be missing the optimal window to detect a difference in the enhancement characteristics of prostate cancer and benign tissue. Although there was no statistical difference between the groups in enhancement over baseline and ADC values, there is a chance that the difference between cancerous and benign tissue may have normalized over time. The majority of prostate cancer in our study was low grade (Gleason 3+3). The utility of detecting low grade prostate cancer is controversial and intermediate grade (Gleason 7) cancers, especially TZ lesions, may benefit from the increased detection as high grade cancers are more easily detected on MRI.Acknowledgements
No acknowledgement found.References
1. Ives EP, Gomella LG, Halpern EJ. Effect of dutasteride therapy on Doppler US evaluation of prostate: preliminary results. Radiology. 2005; 237:197-201.
2. Mitterberger M, Pinggera G, Horninger W, et al. Dutasteride prior to contrast-enhanced colour Doppler ultrasound prostate biopsy increases prostate cancer detetection. European Urology. 2008; 53:112-117.
3. Halpern EJ, Gomella LG, Forsberg F, et al. Contrast enhanced transrectal ultrasound for the detection of prostate cancer: A randomized, double-blinded trial of dutasteride pretreatment. Journal of Urology. 2012; 188:1739-1745.
4. Robertson NL, Moore CM, Ambler G, et al. MAPPED study design: a 6 month randomized controlled study to evaluate the effect of dutasteride on prostate cancer volume using magnetic resonance imaging. Contemporary Clinical Trials. 213; 34:80-89.
Figures