1013
MRI guided biopsy in Patients with positive TRUS-biopsy: Necessity or Overkill?1Radiology, Emory University-School of Medicine, Atlanta, GA, United States, 2Urology, Emory University-School of Medicine, Atlanta, GA, United States, 3Pathology, Emory University-School of Medicine, Atlanta, GA, United States
Synopsis
TRUS biopsy (TRUS-Bx) is the standard of care for prostate cancer diagnosis but has several limitations. Multiparameteric MRI and MRI guided biopsy (MRGB) show considerable added benefits with better disease detection and stratification. The purpose of this study is to evaluate the role of in-bore MRI guided biopsy in patients with positive TRUS-Bx. 40 patients with 71 TRUS-Bx positive lesions were analyzed for cancer detection rate, false negative rate, and Gleason score upgrade by MRGB. MRGB showed 65% cancer detection rate, 35 % false negative rate, and upgraded disease status in 40% of the whole sample
Introduction and Purpose:
TRUS guided prostate biopsy (TRUS-Bx) is the standard of care for prostate cancer diagnosis and active surveillance. It is well known for its limitations as having low cancer detection rates, 1, 2 underestimation of Gleason score 3, 4 and poor sampling to anterior gland lesions. 5 Compared to this traditional approach, in-bore MRI-guided biopsy (MRGB) showed better overall cancer detection, detection of clinically significant cancers, and tumor grading accuracy nearly approaching those of post-prostatectomy histopathology results.6-10 We hypothesize that MRGB provides valuable additional clinical information among patients with a prior positive TRUS-Bx. The purpose of this study is to evaluate the outcomes of MRGB after positive TRUS-Bx in terms of 1) overall cancer detection rate; 2) false negative MRGB (vs TRUS-Bx results); and 3) incidence of Gleason upgrading and detection of new tumors on MRGB .Methods:
Fifty patients with positive TRUS-Bx who underwent subsequent MRGB were retrospectively evaluated. We excluded 10 patients with negative MRGB due to history of treatment after TRUS biopsy. Thus, the final analyzed cohort includes 40 patients with 71 TRUS-Bx positive prostate lesions. All patients had mpMRI with our institutional protocol (T2, DWI and DCE) and transrectal in-bore MRGB using 3T magnet (Magnetom Trio, Siemens, Germany). We compared biopsy results of MRGB and the prior TRUS-Bx. The sites of positive TRUS–Bx were correlated to MRI findings by an experienced radiologist (18 years of experience). Clinically significant cancer was defined as tumor foci with Gleason score ≥ 7. Gleason score upgrade analyzed on both patient (“overall disease upgrade”) and lesion basis. Prostate volumes were categorized into ≤40 vs >40 cc. Categorical variables were interpreted as frequencies and percentages. Quantitative variables were summarized as median and range. Statistical significance is defined as p-value <0.05 tested by Fisher’s exact test for categorical variables and Mann-Whitney U test for quantitative variable. Data were analyzed by SPSS (version 23, IBM) for Microsoft Windows.Results:
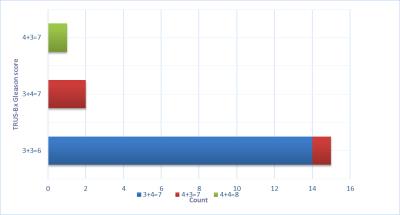
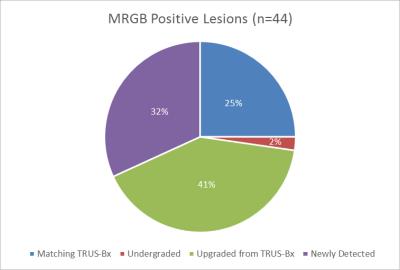
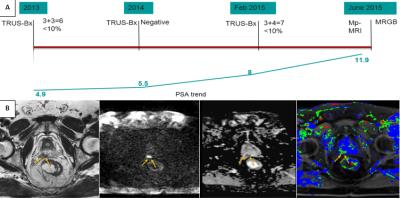
The overall cancer detection rate of MRGB was 65%. MRGB missed 35% (n=14/40) of cases (false negative). Out of the 14 false-negative cases, only three had clinically-significant cancer noted on TRUS-Bx (GS 3+4=7 (Grade group (GG) 2 ) (2 , 14 %) and 4+3=7 (GG 3) (1 ,7%)). Out of all patients in the sample, the overall disease upgrade by MRGB was 40% (16/40) which represents 61.5% (16/26) of the MRGB positive cases (87.5 % from low to intermediate risk, 12.5 % from intermediate to high risk). MRGB under-graded one case from intermediate risk (3+4=7(GG 2)) to low risk (3+3=6 (GG 1)) (3.8%, 1/26). Out of the 71 TRUS-Bx positive lesions, 80% (57/71) had corresponding visible targets on MRI and 20% (14/71) of lesions detected by TRUS-Bx had no image correlates on MRI. Out of TRUS-Bx lesions with corresponding visible targets on MRI, MRGB detected 52.6% (30/57) and missed 47.4% (27/57). Out of the detected lesions, MRGB upgraded about 60% (18/30) (figure 1), and under-graded 3.3% (1/30). Patients with prostate volume >40 cc were more likely to have false negative MRGB (P=0.04). MRGB detected 14 new cancers not detected by TRUS-Bx with grades 3+3=6 (GG 1) (6/14, 42.8%), 3+4=7 (GG 2) (6/14, 42.8%), 4+3=7 (GG 3) (1/14, 7%) and 4+5=9 (GG 5) (1/14, 7%). There was no association of lesions’ size, location, interval between TRUS-Bx and MRGB, level of suspicion and presence of inflammation with false negative results.Conclusion:
MRGB upgraded Gleason scores in patients with a previous positive TRUS-Bx on both patients’ basis (61%) and lesions’ basis (60%). Most of false negative cases had clinically insignificant prostate cancers. The high incidence of disease upgrade resulting from in-bore MRGB following positive TRUS biopsies detected in this study may justify the utilization of MRI guided prostate biopsy for better risk stratification in patients previously diagnosed with low-risk prostate cancer using TRUS biopsy.Acknowledgements
No acknowledgement found.References
1.Presti JC, Jr., O'Dowd GJ, Miller MC, Mattu R, Veltri RW. Extended peripheral zone biopsy schemes increase cancer detection rates and minimize variance in prostate specific antigen and age related cancer rates: results of a community multi-practice study. J Urol. 2003;169(1):125-9.
2.Hricak H, Choyke PL, Eberhardt SC, Leibel SA, Scardino PT. Imaging prostate cancer: a multidisciplinary perspective. Radiology. 2007;243(1):28-53.
3.Hambrock T, Hoeks C, Hulsbergen-van de Kaa C, Scheenen T, Futterer J, Bouwense S, et al. Prospective assessment of prostate cancer aggressiveness using 3-T diffusion-weighted magnetic resonance imaging-guided biopsies versus a systematic 10-core transrectal ultrasound prostate biopsy cohort. Eur Urol. 2012;61(1):177-84.
4.Divrik RT, Eroglu A, Sahin A, Zorlu F, Ozen H. Increasing the number of biopsies increases the concordance of Gleason scores of needle biopsies and prostatectomy specimens. Urol Oncol. 2007;25(5):376-82.
5.Ouzzane A, Puech P, Lemaitre L, Leroy X, Nevoux P, Betrouni N, et al. Combined multiparametric MRI and targeted biopsies improve anterior prostate cancer detection, staging, and grading. Urology. 2011;78(6):1356-62.
6.Overduin CG, Futterer JJ, Barentsz JO. MRI-guided biopsy for prostate cancer detection: a systematic review of current clinical results. Curr Urol Rep. 2013;14(3):209-13.
7.Paulson DF. Impact of radical prostatectomy in the management of clinically localized disease. J Urol. 1994;152(5 Pt 2):1826-30.
8.Coogan CL, Latchamsetty KC, Greenfield J, Corman JM, Lynch B, Porter CR. Increasing the number of biopsy cores improves the concordance of biopsy Gleason score to prostatectomy Gleason score. BJU Int. 2005;96(3):324-7.
9.Steinberg DM, Sauvageot J, Piantadosi S, Epstein JI. Correlation of prostate needle biopsy and radical prostatectomy Gleason grade in academic and community settings. Am J Surg Pathol. 1997;21(5):566-76.
10.Geller RL, Nour SG, Osunkoya AO. Pathologic findings in patients with targeted magnetic resonance imaging-guided prostate needle core biopsies. Int J Clin Exp Pathol. 2015;8(9):9790-5.
Figures