Jian Jiang1, Huihui Wang1, and Xiaoying Wang1
1Peking University First Hospital, Beijing, People's Republic of China
Synopsis
This study is to assess the
factors influencing multiparametric (MP) MR Imaging occuracy in estimating the
volume of clinically significant prostate cancer (Vh) by using
whole-mount step-section slides as standard of reference.
Purpose
To assess the factors influencing
multiparametric (MP) MR Imaging occuracy in estimating the volume of clinically
significant prostate cancer (Vh) by using whole-mount step-section
slides as standard of reference.Methods
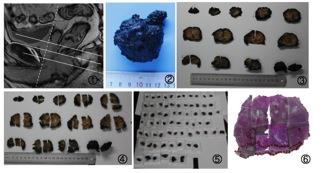
Thirty-six consecutive patients with biopsy-proven
prostate cancer (PCa) were included. All patients received mpMRI of the
prostate, including T2WI, DWI, ADC and DCE. Following radical prostatectomy,
all specimens were processed as whole-mount step-section slides. MR images were
interpreted according to PI-RADS v2 by an experienced radiologist who was
blinded to clinical details and histopathology. Volumes of MR lesions were
measures on T2WI (VT2), on DWI (VDWI), on ADC maps (VADC),
and on DCE (VDCE). The Vh and the MR-derived tumor
volumes were compared by Mann-Whitney
U test, and the correlations between these were computed by using
Spearman coefficients. Generalized linear mixed models were used to test the
influence on MP MR imaging accuracy of the tumor Gleason score, Vh, PI-RADS score.Result
Thirty-six consecutive patients with forty-one clinically
significant cancers (thirty-one peripheral zone (PZ) prostate cancers and ten transitional
zone (TZ) prostate cancers) were included. The Vh had no
statistically significant difference with the other mpMRI’s volumes, but not
with the VDCE (P = .012)
compared with the Vh of PZ prostate cancers. The Vh of PZ
prostate cancers showed strong correlation with VDCE (R2 =
0.735, P < .0001).
The Vh of TZ prostate cancers showed strong correlation with VT2 (R2 = .733, P = .016). At
generalized linear mixed analysis, Vh (P = .015) significantly influenced VDCE of PZ prostate cancers
accuracy. This accuracy was good in tumors with Vh less than 0.5cc. PI-RADS score (P < .0001) and Vh (P < .0001) significantly influenced VT2 of TZ prostate cancers accuracy. This accuracy was good in tumors with PI-RADS score of 5 or Vh less than
0.5cc. Discussion
This study divided the tumor into PZ prostate cancers and TZ prostate cancers based on the
tumor’s locations, and the result emphasized the need to assess the factors influencing MP MR imaging
occuracy before using any MR-derived volume as a surrogate for Vh. As a consequence, this study assessed a model
taking into account not only VDCE of PZ prostate cancers and VT2 of TZ prostate cancers but also the PI-RADS score of the TZ tumors
could improve Vh estimation.Conclusion
Vh can be estimated by using VDCE of PZ prostate cancers, and Vh or the tumors with PI-RADS score of 5 can be estimated by using VT2 of TZ prostate cancers.Acknowledgements
No acknowledgement found.References
No reference found.