1007
PI-RADS Version 2: Preoperative Role in the Detection of Normal-sized Pelvic Lymph Node Metastasis in Prostate Cancer1Radiology, Yonsei University College of Medicine, Seoul, Korea, Republic of
Synopsis
Although the identification of pelvic lymph node metastasis (PLNM) is important in prostate cancer, sometimes PLNM are often not so enlarged on imaging. Therefore, we were trying to identify normal sized PLNM through PI-RADS v2 scores of 221 patients with prostate cancer. In our study, a threshold of PI-RADS v2 score of 5 seems to be associated with an increased risk of normal-sized PLNM, which may help identify the need for further node-specific imaging studies or pelvic lymph node dissection when a patient with prostate cancer has only normal-sized pelvic lymph nodes on preoperative imaging.
PURPOSE
Pelvic lymph node metastases (PLNM) in prostate cancer (PCa.) are often small on preoperative imaging 1. Based on recent studies, a higher Prostate Imaging Reporting and Data System version 2 (PI-RADSv2) score seems to be associated with higher tumor stage, Gleason score (GS), or biochemical recurrence 2-4. Accordingly, it is hypothesized that PI-RADSv2 score may also be associated with the risk of PLNM in PCa. Because mpMRI is now widely accepted as a preoperative diagnostic modality, the identification of normal-sized PLNM with mpMRI may be useful in the selection of patients who need additional node-specific imaging or PLND. The purpose of this study is to analyze whether PI-RADSv2 scores are associated with the risk of normal-sized PLNM in PCa.METHODS
A consecutive series of 221 patients who underwent magnetic resonance imaging and radical prostatectomy with pelvic lymph node dissection (PLND) for PCa were included. No patients had enlarged (≥ 0.8cm in short-axis diameter) lymph nodes. Clinical parameters [prostate-specific antigen (PSA), greatest percentage of biopsy core, and percentage of positive cores] and PI-RADSv2 score from two independent readers were recorded. Logistic regression, receiver operating characteristic curve and weighted kappa were used.RESULTS
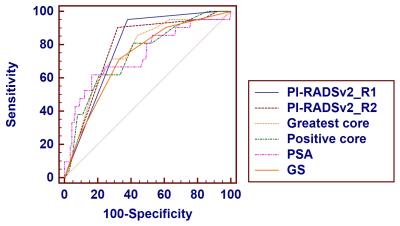
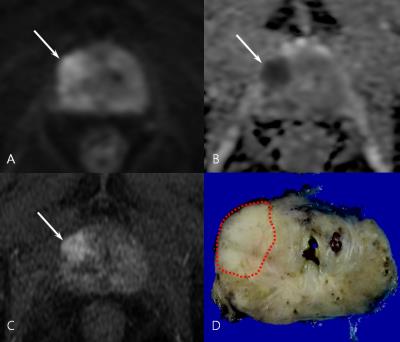
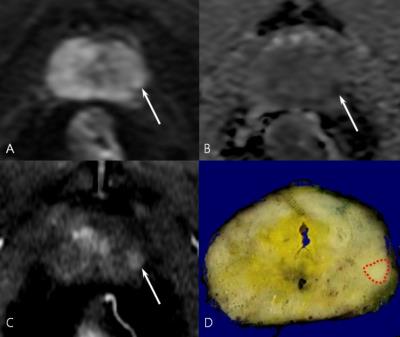
Normal-sized PLNM was found in 9.5% (21/221) of patients. The area under the curve of PI-RADSv2 for normal-sized PLNM was 0.788 (95% confidence interval [C.I.], 0.728-0.840) for reader 1 and 0.786 (95% C.I., 0.726-0.839) for reader 2 (figure 1). In multivariate analysis, PI-RADSv2 (reader 1, OR= 18.465, p= 0.009; reader 2, OR=4.406, p= 0.026) and PSA (reader 1, OR= 1.025, p= 0.008; reader 2, OR= 1.020, p=0.037) were predictive of normal-sized PLNM (figure 3-4). The threshold of PI-RADSv2 was a score of 5, where PI-RADSv2 was associated with high sensitivity (reader 1, 95.2%; reader 2, 90.5%) and negative predictive value (reader 1, 99.2%; reader 2, 98.6%) for normal-sized PLNM. The inter-reader agreement was excellent for PI-RADSv2 of 5 or not (weighted kappa= 0.804).DISCUSSION
In our study, a threshold of PI-RADSv2 score of 5 seems to be associated with an increased risk of normal-sized PLNM, which may help identify the need for further node-specific imaging studies or pelvic lymph node dissection when a patient with prostate cancer has only normal-sized pelvic lymph nodes on preoperative imaging. In addition, the inter-reader agreement was excellent regarding if a PI-RADSv2 score of 5 or not (weighted kappa= 0.804). Thus, our initial report may widen the field of PI-RADSv2 application, especially as a reproducible imaging biomarker for the selection of optimal candidates who need advanced nodal imaging studies or pelvic lymph node dissection in prostate cancer. To the best of our knowledge, this is the first report to demonstrate clinical usefulness of PI-RADSv2 for assessing normal-sized PLNM in prostate cancer.CONCLUSION
PI-RADSv2 scores may be associated with the risk of normal-sized PLNM in PCa.Acknowledgements
No acknowledgement found.References
1. McMahon CJ, Rofsky NM, Pedrosa I Lymphatic metastases from pelvic tumors: anatomic classification, characterization, and staging. Radiology. 2010;254:31-46.
2. Vargas HA, Hotker AM, Goldman DA, et al. Updated prostate imaging reporting and data system (PIRADS v2) recommendations for the detection of clinically significant prostate cancer using multiparametric MRI: critical evaluation using whole-mount pathology as standard of reference. Eur Radiol. 2016;26:1606-1612.
3. Kayat Bittencourt L, Litjens G, Hulsbergen-van de Kaa CA, et al. Prostate Cancer: The European Society of Urogenital Radiology Prostate Imaging Reporting and Data System Criteria for Predicting Extraprostatic Extension by Using 3-T Multiparametric MR Imaging. Radiology. 2015;276:479-489.
4. Park SY, Oh YT, Jung DC, et al. Prediction of biochemical recurrence after radical prostatectomy with PI-RADS version 2 in prostate cancers: initial results. Eur Radiol. 2016;26:2502-2509.
Figures