0979
Feasibility of magnetic resonance colonography for an immune check-point inhibitor in orthotopic colorectal rechallenge tumor models1Asan Institute for Life Sciences, ASAN Medical Center, Seoul, Korea, Republic of, 2Medical research institute, Gangneung Asan Hospital, Gangneung, Korea, Republic of, 3Department of Radiology, ASAN Medical Center, Seoul, Korea, Republic of
Synopsis
In the immunotherapy research field, establishing appropriate preclinical model is very important to evaluate the complex immune reaction. Orthotopic tumor model is more physiologic than ectopic tumor model, however its use may be limited due to difficulty in evaluating deep-seated tumors, especially in the colorectum having a complex anatomy. MR colonography (MRC) is a new technique in preclinical trial, which uses Fluorinert, a negative contrast agent, to fill the colorectum. Our study demonstrated that MRC is quite feasible to evaluate colorectal tumors and metastatic foci in orthotopic colorectal tumor model, which can be useful in immunotherapy drug development.
Purpose
In the immunotherapy research field, it is important to evaluate the immunity at the orthotopic tumor site rather than ectopic site. To monitor the deep-seated orthotopic tumor, MRI is necessary. However, achieving good quality MRI of the colorectum is difficult due to its complex anatomy, thus requiring special MR colonography (MRC) technique. We aimed to assess the feasibility of MRC technique to evaluate efficacy of an immune check-point inhibitor in an orthotopic colorectal rechallenge tumor model.Materials & Methods
Rechallenge tumor model and anti-PD-L1 administration: Anti-PD-L1 antibody (PD-L1 mAb) was generously gifted by Scripps Korea Antibody Institute. The orthotopic rechallenge tumor model was generated as follows: (1) 1x106 MC38 cells were implanted into the subcutaneous layer of C57BL/6 mice (male, 8 weeks old), (2) mice were randomly allocated into control group and PD-L1 group, (3) total four times of either saline or 10mg/kg PD-L1 mAb were administered in control group and PD-L1 group, respectively (n=5 for each group), every three days since 7th day post implantation, and (4) on 21th day post implantation, subcutaneous tumor was resected and 1x105 MC38 cells were subsequently engrafted in the rectum. Mice were sacrificed after 14 days after tumor rechallenge.
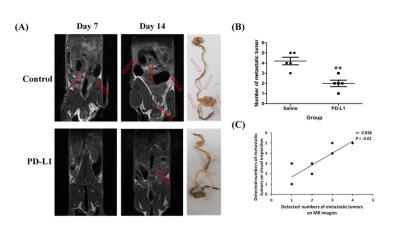
Magnetic resonance colonography technique: We used MRC technique to monitor colorectal tumor, i.e., rechallenge tumor, and its metastatic foci [1]. At first, a cleansing enema was performed using 150 μl of saline. The colon was then subsequently filled with Fluorinert which does not produce any MR proton signal. Contrast-enhanced T1-weighted images (CE-T1w) of all surviving mice were acquired using a 9.4T MRI scanner (Agilent, Inc.) at 7 and 14 days after tumor rechallenge. Gadoterate meglumine (Guerbet, Paris, France) was used as an intravenous contrast agent. Volumtery of the rechallenge tumors was done by multiplying the summed area of all tumor areas by the slice thickness. The numbers of metastatic tumor foci were counted on MR images and in the gross histologic specimens.
Histologic evaluation: Using specimens of extracted rechallenge tumors and metastatic tumors, hematoxylin and eosin (H&E) stain and multiplex immunohistochemistry (IHC) with antibodies to target CD4 and CD8 of T-cells were performed. On IHC stain, the degree of immune cell infiltration was analyzed by calculating the percentage of CD4 or CD8 positive areas per unit area of tumor using a confocal microscope (LSM 780, Zeiss, Germany).
Statistical analysis: Between the control group and PD-L1 group, we compared volumetry results of rechallenge tumors, numbers of metastatic foci, and immune cell infiltration degree using two-tailed Student's t-test. To test the reliability of metastatic tumor detection between MRC and visual inspection on gross specimen, the Pearson correlation coefficient was calculated.
Results
In all MRC images, excellent distension of the colorectum was achieved by Fluorinert insertion, which enabled us to discriminate the colon and tumor (Fig. 2A, 2B). Thus, we were able to perform the volumetry for the rechallenge tumor and count the number of metastatic tumors in all mice. The measured volume of rechallenge tumor was significantly lower in PD-L1 group than control group at day 7 (0.18 ± 0.04 vs 0.09 ± 0.02, p<0.05) and day 14 (0.42 ± 0.08 vs 0.22 ± 0.03, p<0.05) (Fig 2C). The number of metastatic tumors was also significantly lower in PD-L1 group than control group (4.40 ± 0.55 vs. 2.20 ± 0.83, p<0.05) (Fig. 3). The strong positive correlation in number of detected metastatic tumors was observed between MRC and visual inspection on gross specimen (r=0.836, p<0.01). This indicates that the detectability of MRC to find the metastatic foci is comparable with that of visual inspection. On H&E stain, the rechallenge tumors and metastatic foci were histologically confirmed (Fig. 4A). On IHC stain, the degree of CD4+ cell infiltration was greater in PD-L1 group than in control group in both rechallenge tumors (0.083 ± 0.025 vs. 0.020 ± 0.003, p<0.01) and metastatic tumors (0.503 ± 0.048 vs. 0.064 ± 0.017, p<0.001). The degree of CD8+ cell infiltration between PD-L1 group and control group differed significantly in metastatic tumors (0.229±0.012 vs. 0.001±0.000, p<0.001), but did not differ in rechallenge tumors (0.001±0.000 vs. 0.001±0.000, p>0.05).Discussion
The present study demonstrated that MRC is quite feasible to evaluate colorectal tumors and metastatic foci in orthotopic tumor model. MRC was accurate in measuring the size of colorectal tumors and counting the metastatic foci, when comparing histological analysis. Thus, MRC can be very useful in orthotopic colorectal tumor model, of which importance has been increasing in immunotherapy research field.Acknowledgements
No acknowledgement found.References
[1] Lilia V. et al. Nature protocol , 2014, 9.11 : 2682-2692.
[2] Ohaegbulam K. C. et al. Trends in molecular medicine, 2015, 21.1 : 24-33.
[3] Koyama S. et al. Nature communications. 7.
[4] Vebrugge, I et al. Cancer research, 2012, 72.13 : 3163-3174.
[5] Reardon D. A. et al. Cancer immunology research, 2015, canimm-0151.
Figures