0977
High resolution imaging of the optic chiasm at 7T MRI improves lesion detection and tumour delineation compared to 3T1Radiology, LUMC, Leiden, Netherlands, 2Radiology, CJ Gorter center for high field MRI, LUMC, Leiden, Netherlands, 3Ophthalmology, LUMC, Leiden, Netherlands, 4Neurosurgery, LUMC, Leiden, Netherlands, 5Endocrinology, LUMC, Leiden, Netherlands
Synopsis
The limited resolution of 3Tesla MRI often leads to missed lesions or ambiguities in the tumour environment for patients with a pituitary macro-adenoma. In this study we developed a robust high-resolution 7Tesla MRI-protocol of the optico-chiasmatic system and evaluated its clinical value. The 7T MR-images reveal tiny lesions in the optic nerve or chiasm which are not visible at 3T. These lesions could explain the vision loss for 3 of the 7 evaluated patients and gave the physician new treatment possibilities. Overall, this study shows the great clinical opportunities of 7Tesla MRI for patients with pituitary macro-adenoma or other neuro-ophthalmic conditions.
Introduction
Patients with a macro-adenomas of the pituitary gland often suffer from visual problems, such as visual field losses, because the tumour compresses the optic chiasm.1 Surgical removal of the tumour often restores most of the visual function.
3T MRI is used as the main imaging technique in the diagnosis, surgical planning and post-surgery follow-up of patients with pituitary adenomas. MRI is used preoperatively to assess the morphology of the tumour and optic chiasm, while the post-operative scans are used to detect any residual adenomas, as well as larger lesions involving the optic chiasm.
However, for some questions rising in the process of diagnosis and treatment, the spatial resolution/signal-to-noise of the 3T MRI technique is inadequate.2 In preoperative planning it is sometimes hard to judge whether a lesion touches the chiasm or not. Furthermore, in a number of patients the vision problems reoccur years after successful surgery, while no abnormalities can be seen on the 3T MRI.
Although higher spatial resolution and signal-to-noise are possible at 7T than at 3T, there are also increased sensitivities to motion and magnetic susceptibility artefacts. The presence of air-tissue and air-bone transitions in the area of the optic chiasm are potentially problematic.3 Therefore, the aim of the study was to determine in a clinical setting whether the advantages of the higher field outweighed the disadvantages in a true patient population.
Purpose
To develop a robust high-resolution protocol
for imaging the optic chiasm and optic nerves on a 7T scanner, and determine to
what degree it has additional value in the diagnosis and treatment of patients
with pituitary macro-adenomas compared to conventional 3T imaging.
Methods and materials
Images were acquired on a Philips 3 T and Philips 7T Achieva
systems using a 32-channel head coil. The
standard clinical protocol was run on the 3T system, and protocols based on the
same sequences were optimized on the 7T (3D T1-weighted gradient-echo:
TE/TR/flip-angle:2.1ms/4.9ms/7°, resolution:(0.7mm)3,
FOV:246x246x100mm3, time: 4:50min; three orthogonal 2D T2-weighted
spin echo: TE/TR:61ms/3403ms, resolution:0.45x0.45x1.0mm3, FOV: 140x180x24mm3,
time:7:43min. For the transverse scan SPAIR fat-suppression was added,
increasing the TR to 4000ms and scan time to 8:16min). Third order shimming was
performed on a localized volume of interest before image acquisition. A total
of 7 patients were scanned on both systems.
Results
The scan protocol developed on the 7T scanner proved to be robust for each of the patients scanned, with image quality superior to the 3T:no magnetic susceptibility artefacts were seen which would interfere with clinical diagnosis.
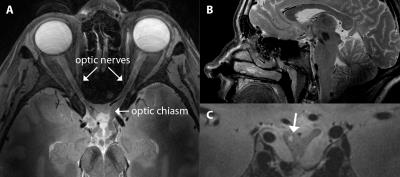
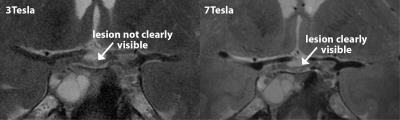
In one patient, a small lesion in the optic nerve was seen on the 7T T2-weighted images due to the higher resolution, which was not visible on the 3T images (Figure 1(a) and (b)). In another patient the ability to acquire much thinner slices (1 mm vs. 3 mm) with adequate signal-to-noise showed that the tumour was actually in physical contact with the chiasm (Figure 2(a)), whereas in the partial-volume averaged 3 mm slice acquired at 3T this was not apparent. In a third patient, a tiny lesion in a heavily deformed chiasm was seen at 7T which was not visible at 3T (Figure 3(c)).
Discussion
For three of the seven patients studied so far, the higher resolution of the 7Tesla MRI provided a direct clinical benefit, representing a significant percentage of patients studied. In one of the preoperatively scanned patients, the 7Tesla MRI clearly showed a tumour touching the chiasm, which was not apparent from the 3T Images. This information was key for the neurosurgeon to plan the best approach for the intervention. It could potentially also allow for a better prediction of the post-operative visual function.
In general, 3T MR images do not have sufficient resolution
to reveal a potential cause for the visual field defects patients develop after
a successful treatment. This was also the case for the patients from this study.
For two of those patients, however, the 7T MRI showed a tiny lesion in either the
optic nerve or optic chiasm. The location of the lesions corresponded to the
observed visual field defects. This was an important confirmation for the
ophthalmologist to develop a treatment strategy.
Conclusion
The increased resolution of
7Tesla MRI reveals tiny lesions in the optico-chiasmatic
system which are not visible at 3T. This provides direct clinical
opportunities for the treatment of patients with pituitary tumours and other
neuro-ophthalmic conditions.
Acknowledgements
No acknowledgement found.References
1. Ogra, S. et al. Visual acuity and pattern of visual field loss at presentation in pituitary adenoma. J Clin Neurosci 21, 735–740 (2014).
2. Pereira, A. M., Biermasz, N. R. Treatment of nonfunctioning pituitary adenomas: What were the contributions of the last 10years? A critical view. Annales d'Endocrinologie 73, 111–116 (2012).
3. de Rotte, A. A. J. et al. High resolution pituitary gland MRI at 7.0 tesla: a clinical evaluation in Cushing's disease. Eur Radiol 26, 271–277 (2016).
Figures
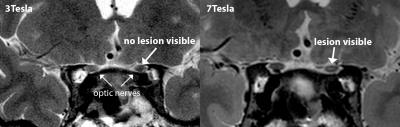
Figure 1: T2-weighted MR-images of a patient who developed visual field defects 4 years after a successful pituitary tumour treatment. On the 7T images a hyperintense lesion in the optic nerve is clearly visible, which is not visible on the conventional 3T images. The location of the lesion corresponded with the location of the visual field defects.
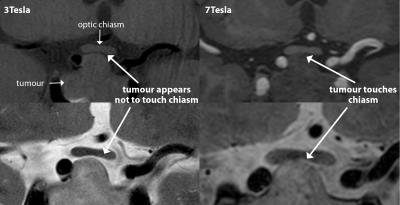
Figure 2: T1 (upper) and T2 (lower) pre-operative MR-images of a patient with a large pituitary macro-adenoma. The 7T images, with 1mm slice thickness, clearly show physical contact between the tumour and optic chiasm, which was not apparent in the 3T images, with 3mm slice thickness, due to partial-volume averaging. This information was key for the neurosurgeon as he could take the physical contact into account during the planning of the best approach for the intervention.