0948
B1 Mapping for Breast Sodium MRI at 7T- A Comparison between Double Angle and Phase-sensitive Method1Department of Biomedical Imaging and Image-guided Therapy, Medical University of Vienna, Vienna, Austria, 2Christian Doppler Laboratory for Clinical Molecular MRI, Christian Doppler Forschungsgesellschaft, Vienna, Austria, 3Research Unit of Medical Imaging, Physics and Technology, University of Oulu, Oulu, Finland, 4Institute of Radiology, University Hospital Erlangen, Erlangen, Germany, 5Division of Medical Physics in Radiology, German Cancer Research Centre (DKFZ), Heidelberg, Germany
Synopsis
Absolute values of sodium content in tumors is one of the most important biomarkers for cancer diagnostics and therapy monitoring. An accurate quantitative values are influenced by B1 inhomogeneity that must be evaluated and corrected. In this work, we compared two mapping methods DAM and PS. On the basis of our results, we found that DAM gives overestimated flip angle values (approximately 30% higher than PS). Also, after correction is applied, DAM shows higher signal drop in comparison with PS. Accompanied with longer measurement time necessary for DAM, this findings give advantages to PS in clinical studies and routine implementation.
PURPOSE:
METHODS:
Sodium B1 maps were obtained in a saline breast shaped phantom (154 mM saline solution, completely filling the coil volume) and eight healthy volunteers (mean age 32±7 years) to verify the technique in vivo. The experiments were approved by the institutional review board. The scans were performed on a 7T whole-body system (Siemens, Erlangen, Germany) using dual-tuned sodium/proton breast coil (QED, 14 23Na channels; two 1H channels; QED, OH, USA). Images for DAM were acquired using a density-adapted, three dimensional radial projection reconstruction sequence (3DPR) with following parameters: flip angle α=45° and 90°,TR/TE = 225/0.7 msec, matrix size = 128×128, 7000 projections and scan time of ~20 min for each set of images (3). For PS mapping, we used double pulse sequence (4) with TR/TE = 410/0.50 ms, 1500 projections, pulse durations of 4000 and 1900 µs and with overall measurement time ~10 min. B0 mapping was performed using double echo 3DPR sequence (TEs of 0.6 and 1.6 ms). For image reconstruction, we used sum-of-squares (SOS) for DAM and adaptive combine (ADC) for PS. For both methods, we employed only Rx/Tx elements of the coil, due to B1+=B1- condition. B1 maps and image corrections were calculated using matlab scripts (Matlab, MathWorks, Natick, MA, USA).RESULTS:
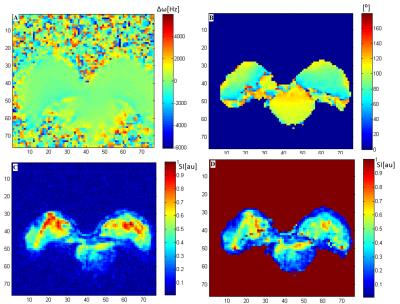
The B1 map from the DAM method calculated based on homogenous phantom data show significantly different values in comparison with PS over the full breast coil volume ( 110±15° vs 85±5° ( p= 0.081)) (Fig. 1-A,1-B). B0 map shows moderate field homogeneity, with Δω<50Hz (Fig. 2A). In phantoms, analyzing the magnitude data from both methods, we found that PS method, after correction is applied, illustrate the higher SNR in comparison to DAM (for PS signal drop after correction was 2.2±0.5% and for DAM 4.8±1.2%) (Fig.1-E, 1-F). DAM was not suitable for signal enhancement correction at the edges of the phantom. After correction, signal enhancement remained 20% of its initial value (Fig. 1-C, 1-E). For in vivo data, we found that PS method is feasible in correction of high signal in retromammary regions of breast, close to the coil walls, keeping the anatomical details intact (Fig. 2-C, 2-D ).DISCUSSION:
An accurate B1 mapping method, which can be performed in clinically acceptable measurement times, has yet to be established. B0 and B1 mapping methods suitable for quantitative 23Na MRI were tested in phantoms and in vivo. Our data demonstrate several advantages of PS method over the DAM. PS was more efficient in signal corrections and SNR preventions. We obtained an overestimated flip angles calculated using DAM which was in agreement with previous work using a single channel RF coil (1). However, this could result in errors in B1-corrected 23Na images and absolute sodium quantifications.CONCLUSION:
PS method was demonstrated as more powerful and accurate in FA mapping and image corrections than DAM. With a clinically feasible time of 10 min, has potential to be implemented in any working protocol for breast 23Na MR imaging.Acknowledgements
We acknowledge financial support by the WWTF project (LS14-096).References
1. Allenet al. Magn. Reson. Med. 2011; 65(4): 1125–1130.
2. Lommen et al. NMR Biomed. 2016; 29: 129–136.
3. Nagel et al. Mag Reson Med 2009; 62:1565-1573
4. Benkhedah et al. Mag Reson Med 2013; 70:754–765.
Figures
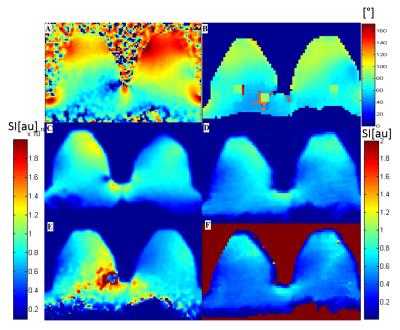
Figure 1. B1 mapping and corrections obtained in saline phantom. Flip angle map calculated using A) DAM and B) PS method. Uncorrected sodium images C) and D). E) Corresponding image corrected by DAM shows high signal intensity in medial part of right breast induced by correction algoritm. Image F) demonstrate more homogenous signal after PS correction and less noise in medial regions.