0914
Multi-Parametric Spinal Cord MRI Detects Subclinical Tissue Injury in Asymptomatic Cervical Spinal Cord Compression1Neurosurgery, University of Toronto, Toronto, ON, Canada, 2Electrical Engineering, École Polytechnique de Montréal, Montréal, QC, Canada, 3Neurosurgery, University of Calgary, Calgary, AB, Canada, 4Medicine, University College Cork, Cork, Ireland, 5Medical Imaging, University of Toronto, Toronto, ON, Canada
Synopsis
Degenerative cervical myelopathy (DCM) involves extrinsic spinal cord (SC) compression causing tissue injury and neurological dysfunction. Asymptomatic SC compression is much more common (8-26%), but it is unknown if tissue injury occurs in this group. Our multi-parametric MRI protocol previously identified 10 measures of tissue injury in DCM. Using these techniques, we demonstrate that asymptomatic SC compression subjects show a similar pattern of tissue injury, with 8/10 measures (p=0.05) showing the same direction of changes and MTRRostral (p=0.002), MTRMCL (p=0.03), and T2*w WM/GMRostral (p=0.04) showing significant univariate differences. A logistic regression model retaining 3 MRI measures shows 86% discrimination between compressed and uncompressed subjects.
INTRODUCTION
Degenerative cervical myelopathy (DCM) is a condition in which extrinsic compression and dynamic injury cause spinal cord (SC) tissue injury and neurological dysfunction. Asymptomatic SC compression occurs much more frequently (8-26%), increasingly with age,1-4 and 25% of these individuals progress to myelopathy within 4 years.5,6 Kerkovsky et al. (2012) used diffusion tensor imaging (DTI) to provide the first evidence that asymptomatic patients experience tissue injury in the compressed cord, showing slightly decreased fractional anisotropy (FA) at the maximally compressed level (MCL) (p=0.04).7 However, this study included subjects with radiculopathy (which sometimes originates within the SC), and DTI metrics can be biased at compressed levels due to susceptibility artefact.
We previously reported results of a multi-parametric MRI protocol to assess cervical SCI tissue injury, demonstrating significant differences between 56 DCM and 32 healthy subjects in 10 metrics.8,9 In the current study, we test the hypothesis that asymptomatic subjects with cervical SC compression experience mild tissue injury that can be detected with the same 10 MRI measures.
METHODS
35 healthy subjects underwent 3T MRI (GE) including T2-weighted (T2w) imaging (FIESTA-C, 0.8x0.8x0.8mm3), diffusion tensor imaging (DTI, ssEPI, 1.25x1.25x5mm3), magnetization transfer (MT; SPGR with/without prepulse, 1x1x5mm3), and T2*-weighted (T2*w) imaging (MERGE, 3 echoes, 0.6x0.6x4mm3) covering C1-C7.8 Subjects were grouped based on presence of cord compression, defined as indentation, flattening, or focal torsion. Cases in which tissues (e.g. disc) contacted the SC without deformation were categorized as uncompressed. Subjects were examined by a physician (ARM) to confirm the absence of neurological symptoms/signs.
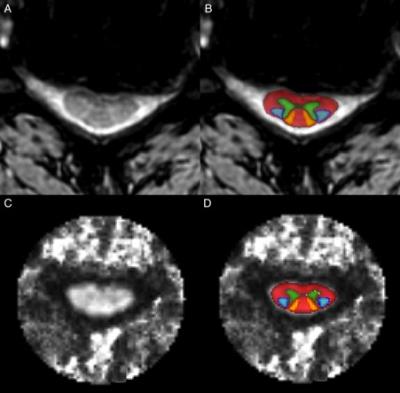
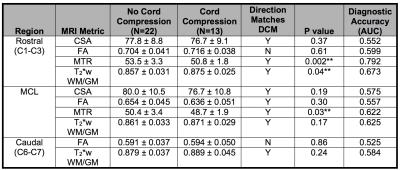
MRI data were analyzed with the Spinal Cord Toolbox (SCT)10 to calculate SC cross-sectional area (CSA), fractional anisotropy (FA), MT ratio (MTR), and T2*w white to grey matter signal intensity ratio (T2*w WM/GM) at the MCL, rostral (C1-C3), and caudal (C6-7) levels and normalized for confounding variables (including age) (Figure 1). The study hypothesis was tested with a single binomial test comparing the direction of changes in 10 measures in compressed subjects with results previously seen in DCM patients, (α = 0.05). Changes in individual metrics were assessed with t tests (without correction for multiplicity). Area under receiver operating characteristic curves (AUC) measured discrimination (diagnostic accuracy) of each MRI measure and logistic regression with backward stepwise variable selection determined multivariate discrimination (maximum 3 degrees of freedom due to sample size).
RESULTS
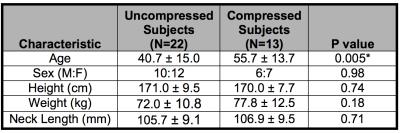
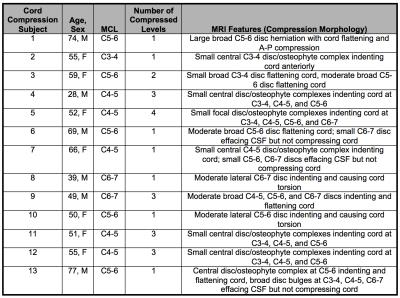
Thirteen subjects (37%) were found to have SC compression, and these were older than uncompressed subjects (age 55.7 vs. 40.7, p=0.005) (Table 1). Cord compression was more frequent among subjects with age ≥ 50 (10/17, 59%) than those under 50 (3/18, 17%). Cord compression occurred at ≥ 2 levels in 6/13 subjects (46%) and at a single level in the remainder, with morphology including indentations (10 subjects), flattening (5 subjects), and torsion (2 subjects) (Table 2).
Overall, compressed subjects showed a similar pattern of tissue injury as previously reported in DCM, with the same direction of differences in 8/10 MRI measures (p=0.05) (Table 3). These differences included significantly decreased MTRRostral (50.8 vs. 53.5, p=0.002) and MTRMCL (48.7 vs. 50.4, p=0.03), and increased T2*w WM/GMRostral (0.875 vs. 0.857, p=0.04). The other 7 metrics did not show significant differences. MTRRostral showed moderately good discrimination between groups with AUC=0.792 while other metrics showed weaker results. A logistic regression model retaining MTRRostral, T2*w WM/GMRostral, and CSAMCL had AUC=0.860.
DISCUSSION
Asymptomatic individuals with SC compression show macro- and microstructural evidence of tissue injury similar to DCM patients, confirming a prior report suggesting the presence of subclinical tissue injury in this group.7 These results offer the intriguing possibility of injury detection prior to the onset of clinical symptoms/signs. Asymptomatic compression had higher prevalence in our data than previously reported, which may relate to a broader definition of cord compression and/or the use of high-resolution isotropic anatomical imaging in our study. CSAMCL only showed a small (non-significant) decrease in compressed subjects, indicating that this group had very mild deformation of the cord. MTR showed the strongest differences suggesting that demyelination may be the predominant mechanism of microstructural changes early in this disease process. This is consistent with our results in DCM where MTR showed significant decreases between mild DCM and healthy subjects but minimal further changes as disease severity increases.9 These findings have far-reaching implications, including the potential for earlier diagnosis and treatment for all spinal pathologies that share common mechanisms of demyelination, axonal injury, and atrophy. Although individual measures did not exceed AUC of 80%, a model with 3 variables improved to 86% and further improvements are likely with more complex multivariate models, confirming the utility of our multi-parametric approach.Acknowledgements
This research received funding support from Rick Hansen Institute, as part of the Riluzole in Spinal Cord Injury Study (RISCIS), which is also supported by AOSpine North America, AOSpine International SCI Knowledge Forum, and the North American Clinial Trials Network (NACTN) of the Christopher and Dana Reeve Foundation. This research also received support from the Dezwirek Foundation, the Sherman Clinical Research Unit, and the Gerald and Tootsie Halbert Chair in Spinal Cord Research. Dr. Martin received post-doctoral fellowship support from Canadian Institutes of Health Research.References
1. Teresi LM, Lufkin RB, Reicher MA, et al. Asymptomatic degenerative disk disease and spondylosis of the cervical spine: MR imaging. Radiology. 1987;164(1):83-8.
2. Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72(8):1178-84.
3. Matsumoto M, Fujimura Y, Suzuki N, et al. MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg Br. 1998;80(1):19-24.
4. Lee MJ, Cassinelli EH, Riew KD. Prevalence of cervical spine stenosis. Anatomic study in cadavers. J Bone Joint Surg Am. 2007;89(2):376-80.
5. Wilson JR, Barry S, Fischer DJ, et al. Frequency, Timing, and Predictors of Neurological Dysfunction in the Nonmyelopathic Patient With Cervical Spinal Cord Compression, Canal Stenosis, and/or Ossification of the Posterior Longitudinal Ligament. Spine. 2013;38(22):S37-S54.
6. Bednarik J, Kadanka Z, Dusek L, Kerkovsky M, Vohanka S, Novotny O, et al. Presymptomatic spondylotic cervical myelopathy: an updated predictive model. Eur Spine J. 2008;17(3):421-31.
7. Kerkovsky M, Bednarik J, Dusek L, Sprlakova-Pukova A, Urbanek I, Mechl M, et al. Magnetic resonance diffusion tensor imaging in patients with cervical spondylotic spinal cord compression: correlations between clinical and electrophysiological findings. Spine (Phila Pa 1976). 2012;37(1):48-56.
8. Martin AR, De Leener B, Cohen-Adad J, Aleksanderek I, Cadotte DW, Fehlings MG. A Clinically Feasible Quantitative MRI Protocol to Assess Tissue Injury in the Cervical Spinal Cord Using DTI, MT, and T2*-Weighted Imaging: Reliability and Variations with Confounding Variables. The Spine Journal. Oct 2016;16(10) Suppl S199–S200.
9. Martin AR, De Leener B, Cohen-Adad J, Aleksanderek I, Cadotte DW, Kalsi-Ryan S, Tetreault L, Crawley A, Ginsberg HJ, Fehlings MG. Microstructural MRI Quantifies Tract-Specific Injury and Correlates With Global Disability and Focal Neurological Deficits in Degenerative Cervical Myelopathy. Neurosurgery. 2016 Aug;63 Suppl 1:165.
10. De Leener B, Lévy S, Dupont SM, Fonov VS, Stikova N, Collins DL, Callote V, Cohen-Adad J. SCT: Spinal Cord Toolbox, an open-source software for processing spinal cord MRI data. NeuroImage. Epub: Oct 5, 2016.
Figures