0869
Diffusion-weighted MRI in the evaluation of posttherapeutic residual masses in lymphoma1Radiology, N.N. Alexandrov National Cancer Center, Minsk, Belarus, 2Chemotherapy, N.N. Alexandrov National Cancer Center, Minsk, Belarus
Synopsis
Residual masses do often present on posttreatment imaging in lymphoma. We conducted prospective study to evaluate diagnostic capabilities of CT, MRI and diffusion-weighted MRI (MRI-DWI) in differentiation residual tumors and non-active posttreatment masses in 40 lymphoma patients. MRI-DWI with visual analysis of apparent diffusion coefficient (ADC) maps was the most effective technique. Quantitative ADC analysis is a promising tool for differentiation of active and non-active residual masses in lymphoma.
Introduction: Currently positron emission tomography combined with computed tomography (PET/CT) is a standard hybrid imaging technique for lymphoma staging and treatment response evaluation. In lymphoma subtypes with low 18-fludeoxyglucose (FDG) avidity CT should be used instead of PET/CT according to international guidelines.1 Residual masses are often present on posttreatment CT with frequency ranging from 41% in non-Hodgkin lymphoma (NHL) to 64% in Hodgkin Lymphoma (HL).2,3 Most of those residual masses are non-active and will decrease in size during follow-up but ultimate decision should be made during restaging to guide further treatment options. According to recent meta-analysis posttreatment FDG-PET scans in patients with lymphoma suffer from a very high number of false-positive FDG-avid lesions. The false-positive proportions were 23.1% for end-of-treatment FDG-PET in HL and 31.5% for NHL.4 Mentioning high ionizing radiation dose delivered to patient during CT and PET/CT scans there is a need for safer and non-invasive imaging technique for tumor response evaluation in lymphoma. Diffusion-weighted MRI (MRI-DWI) was reported to be an effective lymphoma staging technique.5 We aimed to evaluate diagnostic capabilities of MRI-DWI in differentiation residual tumors and non-active posttreatment masses in patients with lymphoma.
Methods: Local ethics committee permission was obtained for the study. Forty previously untreated lymphoma patients were prospective included (21 HL, 19 NHL). Participant’s age ranged from 19 to 76 years, mean age 41.4 years. CT and MRI-DWI of the neck, chest, abdomen and pelvis were performed in all patients before and after complete course of treatment. MRI was performed with of 1.5 T scanner equipped with built-in body coil. Coronal T1-weighted and STIR, transversal DWI and FIESTA images were obtained. Technical parameters for DWI were as the next: TR 4000 ms, TE 67 ms, TI 180 ms, b factor 0 and 800 s/mm2, slice thickness 5 mm, slice gap 1 mm, field of view 480×432, matrix 80×128, number of excitations 6. Total scan time was 34-40 minutes depending on the patient's height. CT scans were performed with standard technical parameters with reconstructed slices thickness of 5 mm. Diagnostic efficacy of CT, MRI without DWI, MRI-DWI with a visual analysis of DWI images (MRI-DWI-b800) and MRI-DWI with visual analysis of the ADC maps (MRI-DWI-ADC) was separately evaluated. Radiological criteria for non-complete tumor response were as the next: lymph nodes larger than 1 cm in short-axis on CT; the same size criterion was used for MRI without DWI; for MRI-DWI-b800 and MRI-DWI-ADC presence of larger lymph nodes and nodal masses was allowed if signal intensity was below or above paraspinal muscles respectively. For complete tumor response no extralymphatic lymphoma lesions should be present. Biopsy or follow-up of minimum 6 months were used as a reference standard.
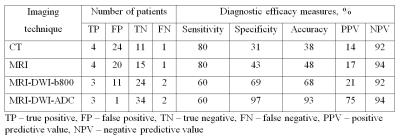
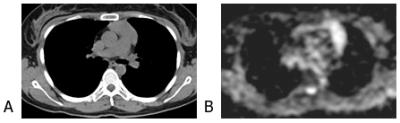
Results: 15 patients (37.5%) were treated with chemotherapy alone, 22 (55%) – with chemotherapy and radiation therapy, 3 (7.5 %) – with standard and high-dose chemotherapy with autologous hematopoietic stem cells transplant. Median follow-up time after treatment was 16.4 months. Non-complete tumor response was established on CT in 28 (70%) patients, MRI – 24 (60%), MRI-DWI-b800 – 14 (35%), MRI-DWI-ADC – 4 (10%). According to reference standard residual tumors were present in 5 (12.5%) patients. Data on diagnostic accuracy of imaging techniques are presented in Fig. 1. Accuracy of MRI-DWI with visual analysis of ADC maps was the highest and that of CT was the lowest. The later was associated with a big number of false-positives as the only CT criterion for non-complete response was the size criterion (Fig. 2).
In 28 patients with residual masses on CT quantitative ADC analysis was performed. One patient was excluded because of small size of residual lesion making ADC measurement difficult. ADC was measured in 27 lymph node lesions before treatment and residual masses after treatment in 25 patients with complete response according to reference standard, and in 8 lymph node lesions before treatment and residual masses after treatment in 2 patients with non-complete response. In complete response group ADC (×10-3 mm2/s) increased from 1.22 to 2.32 (p<0.0005). In patients with active residual tumors ADC not changed – 1.03 and 1.04 respectively (p=0.94).
Conclusion: MRI-DWI with visual analysis of ADC maps is the most effective method compared to CT, MRI without DWI and MRI-DWI with a visual analysis of DWI images in differentiation residual tumors and non-active posttreatment masses in patients with lymphoma. Paraspinal muscles may be used as the reference tissue for visual analysis of DWI images and ADC maps. Quantitative ADC analysis is a promising tool for differentiation of active and non-active residual masses in lymphoma.
Acknowledgements
No acknowledgement found.References
1. Cheson BD, Fisher RI, Barrington SF, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: The Lugano Classification. J Clin Oncol. 2014;32(27):3059-3068.
2. Surbone A, Longo DL, DeVita VT Jr, et al. Residual abdominal masses in aggressive non-Hodgkin's lymphoma after combination chemotherapy: significance and management. J Clin Oncol. 1988;6(12):1832-1837.
3. Radford JA, Cowan RA, Flanagan M, et al. The significance of residual mediastinal abnormality on the chest radiograph following treatment for Hodgkin's disease. J Clin Oncol. 1988;6(6):940-946.
4. Adams HJ, Kwee TC. Proportion of false-positive lesions at interim and end-of-treatment FDG-PET in lymphoma as determined by histology: Systematic review and meta-analysis. Eur J Radiol. 2016;85(11):1963-1970.
5. Balbo-Mussetto A, Cirillo S, Bruna R, et al. Whole-body MRI with diffusion-weighted imaging: a valuable alternative to contrast-enhanced CT for initial staging of aggressive lymphoma. Clin Radiol. 2016;71(3):271-279.
Figures