0860
Differentiating glioma histologic grade preoperatively by two functional modalities: Amide Proton Transfer (APT) and Intravoxel Incoherent Motion (IVIM) MR imaging1Department of Radiology, Zhujiang Hospital, Southern Medical University, Guangzhou, People's Republic of China, 2Philips Healthcare, Guangzhou, People's Republic of China, 3Department of Radiology, Johns Hopkins University School of Medicine, MD, United States
Synopsis
A correct preoperatively grading of glioma is always the most important issue in clinic. APT and IVIM imaging are designed to assess glioma on the level of cell and molecule. So, in this study we combined these two functional techniques hoping to explore their diagnostic performance in differentiating HGG from LGG.
Target audience
Researchers and clinicians who are interested in glioma and functional MR imagingPurpose
Gliomas are the most common primary tumor in CNS1. A correct preoperatively grading of glioma is always the most important issue in clinical settings. Several recent researches2, 3 revealed that linear GBCA gadopentetate dimeglumine prone to deposit in the dentate nucleus and the globus pallidus, and thus may cause healthy risk. APT and IVIM are two novel functional modalities without GBCA. APT imaging is used to detect the amide protons of endogenous, low-concentration mobile proteins and peptides in tissue. IVIM is developed by Le Bihan4 to visualize microscopic motion of water and separate diffusion and perfusion parameters via a single acquisition scheme. There was no research on combining these two techniques in grading glioma. We aimed to investigate the diagnostic performance of APT and IVIM MR imaging in preoperative grading of glioma.Methods
Local Ethics Committee approved the prospective study, and informed consent was obtained from all patients. Fifty-one patients who underwent preoperative routine MRI scan as well as APT and IVIM were retrospectively assessed. All MR scans were performed on a clinical 3.0T scanner (Philips, Achieva, Netherlands). APT imaging was obtained using a fat-suppressed, turbo-spin-echo pulse sequence, with a pulse-train radiofrequency saturation (duration=200ms×4; inter-pulse delay, 10ms; power 2μT). IVIM imaging was based on a diffusion weighted single-shot EPI pulse sequence, with the following parameters: TR/TE=1985/75msec, FOV=230×230 mm2, slice thickness=6mm, reconstruction matrix=192×192, 10 b values 0, 10, 20, 40, 80, 130, 200, 400, 700 and 1000sec/mm2). 4 parameters, amide proton transfer-weighted (APTW), true diffusion coefficient (D), perfusion fraction (f), pseudo-diffusion coefficient (D*), were applied to calculate the solid component at the maximal slice of the tumor and contralateral normal-appearing white matter (CNAWM). All cases were confirmed by postsurgical immunohistochemistry in which 26 were low-grade glioma (LGG) and 25 were high-grade glioma (HGG). Independent-Samples T test and Paired-Samples T test were used to compare differences of 4 parameters between LGG and HGG group. The diagnostic performance of the 4 parameters was assessed with receiver operating characteristic (ROC) curve and area under the curve (AUC).
Results and discussion
APTWtumor, Dtumor were larger than APTWCNAWM and DCNAWM in both groups (P<0.05). For LGG group, there were no statistical difference for f and D* between tumor and CNAWM. While for HGG group, ftumor were significantly higher than fCNAWM, D* reduced obviously in tumor component. Compared to LGG, HGG had higher APTW, ΔAPTW (APTWtumor―APTWCNAWM), f and lower D, the statistical difference between the two groups were significant (P<0.01). (Table 1)
ΔAPTW showed the best performance for discriminating HGG from LGG, followed by APTW. f-value and D showed moderate diagnostic performance, while D* showed lowest diagnostic performance in this study. (Table 2)
Conclusion
APT and IVIM are two promising molecular imaging modalities based on pathophysiologic changing, which could assess glioma on the level of cell and molecule, and provide more precise and microscopic of functional diagnostic information. We believe that these important supplementary methods in clinical settings would be valuable to improve the ability of differentiating low and high grade gliomas.Acknowledgements
References
1. Ostrom Q T, Gittleman H, Fulop J, et al. CBTRUS Statistical Report: Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2008-2012. Neuro Oncol. 2015; 17 Suppl 4: iv1-iv62.
2. Kanda T, Ishii K, Kawaguchi H, et al. High signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted MR images: relationship with increasing cumulative dose of a gadolinium-based contrast material. Radiology. 2014; 270(3): 834-841.
3. Ramalho J, Castillo M, Alobaidy M, et al. High Signal Intensity in Globus Pallidus and Dentate Nucleus on Unenhanced T1-weighted MR Images: Evaluation of Two Linear Gadolinium-based Contrast Agents. Radiology. 2015; 276(3): 836-844.
4. Le Bihan D, Breton E, Lallemand D, et al. MR imaging of intravoxel incoherent motions: application to diffusion and perfusion in neurologic disorders. Radiology. 1986; 161(2): 401-407.
Figures

Table1. Comparing difference of APTW, f, D, D* within LGG and HGG groups
Note: *P<0.05, compare HGG to LGG
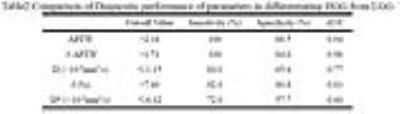
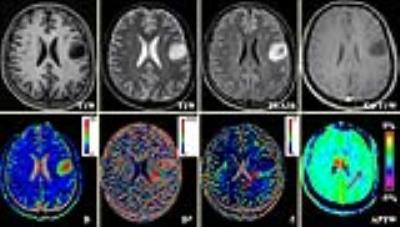
Fig1. APT and IVIM finding in LGG
Figure1: A 24-year-old male with ganglioglioma (WHO II) in the left frontal lobe. The non-Gd-enhanced tumor core has a significant hyperintensity on D-map, while on D*, f and APTW image are relatively homogeneous signal intensity.
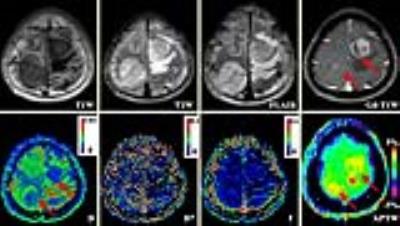
Fig2. APT and IVIM finding in HGG
Figure 2: A 26-year-old male with gliosarcoma in right parietal lobe and left frontal lobe. The non-enhanced mass in right hemicerebrum and obviously-enhanced mass in left side are both hypointensity (6.46-6.98×10-3mm2/s) on D-map and hyperintensity (2.47%-3.12%) on APTW image.