0854
Motion-Sensitized Driven-Inversion (MSDI) for improvement of diffusion-prepared MR neurography (SHINKEI) in the brachial plexus1Philips Electronics Japan, Tokyo, Japan, 2Philips Electronics Australia, North Ryde, Australia, 3Department of Radiological Services, Tokyo Women’s Medical University Hospital, Tokyo, Japan, 4Department of Diagnostic Imaging & Nuclear Medicine, Tokyo Women’s Medical University Hospital, Tokyo, Japan, 5Philips Healthcare AsiaPacific, Tokyo, Japan
Synopsis
Brachial plexus is anatomically complex and may be involved in a variety of pathologies that leads to significant morbidity. MR neurography, based on diffusion-prepared MR neurography (SHINKEI), plays a major role in the diagnostic work-up of plexus pathologies. To solve the problems that caused by the current fat suppression techniques (SPAIR and STIR) with SHINKEI, we developed motion-sensitized driven inversion (MSDI). MSDI could simultaneously suppress fat, flow and muscle signals using only one pre-pulse module. SHINKEI with MSDI provides uniform fat suppression in the brachial plexus, as in STIR, with no significant decrease in SNR compared to SPAIR.
Purpose
The brachial plexus is anatomically complex and may be involved in a variety of pathologies that leads to significant morbidity. MR neurography plays a major role in the diagnostic work-up of plexus pathologies, substantially improving early diagnosis and patient management1-3.
Recently, we proposed a diffusion-prepared MR neurography sequence (nerve-SHeath signal increased with INKed rest-tissue RARE Imaging: SHINKEI)4. By using this sequence, high-quality MR neurography has been obtained in the brachial plexus and the lumbosacral plexus2-5. SHINKEI can be combined with different types of fat saturation techniques. Spectral attenuated inversion recovery (SPAIR) or short tau inversion recovery (STIR) are frequently used in the brachial plexus. Although SPAIR-SHINKEI facilitates excellent visibility of the nerves with high signal-to-noise ratio (SNR), image quality is often compromised by poor fat suppression. The origin of failed fat suppression can be found in poor homogeneity of the magnetic field (B0), which is mainly caused by susceptibility differences between air and tissue around the neck6. Although B0 image-based shimming can be applied, this still results in suboptimal homogeneity using standard shimming routines only3. On the other hand, STIR-SHINKEI provides uniform fat suppression; however, it suffers from significant decrease of SNR of the nerves compared with SPAIR-SHINKEI6.
To solve these problems caused by the fat suppression technique, we developed a new pre-pulse, motion-sensitized driven inversion (MSDI), to improve the image-quality of SHINKEI MR neurography in the brachial plexus.
Methods
Theory and pulse sequence:
Fig.1 shows the differences between MSDE and MSDI. MSDE is based on the improved MSDE (iMSDE)7, where additional eddy-current compensation is adopted in front of 90-degree pulse8. In MSDI the phase of the final 90-degree pulse is inverted.
Conventional SHINKEI consists of both fat suppression IR (SPAIR or STIR) and MSDE preparation, with a 3D T2-weighted TSE sequence to acquire the data. The MSDE module has a long duration to suppress flow and muscle signal simultaneously4 [Fig.2a]. MSDI-prepared SHINKEI uses only one pre-pulse module, but this can suppress the fat tissues by inverting the fat signals due to the final 90-degree pulse. Consequently, MSDI enables the suppression of fat, flow and muscle signals simultaneously [Fig.2b].
Experiments:
A total of five volunteers were examined on 3.0T systems (Ingenia, Philips Healthcare). The study was approved by the local IRB, and written informed consent was obtained from all subjects.
(1) Parameter optimization of MSDI-SHINKEI
To optimize the scan protocol of MSDI-SHINKEI for the brachial plexus, firstly we investigated the optimal MSDI delay time for suppressing fat signals. Subsequently we compared the two types of adiabatic refocusing pulses (the conventional hyperbolic secant and a broadband offset independent trapezoid) to stabilize the depiction of the nerves over the full field-of-view (FOV).
(2) Comparison of MSDI-SHINKEI with conventional SPAIR/STIR methods
To validate the quality of neurography images obtained by MSDI-SHINKEI, coronal brachial plexus images were acquired and were quantitatively compared with conventional methods. Neurography images were compared with conventional SHINKEI with SPAIR/STIR for image quality. We measured/calculated the SNR of the nerves (average value of both the left and right dorsal root ganglion from C5 to C8) by using noise measurement method9. The SNR were assessed by using one-way repeated measures analysis of variance and the post-hoc Tukey test. The imaging parameters common to all methods were: TR=2500ms, TE=63ms, ETL=100, echo spacing=4.0ms, voxel size=1x1x1mm3, 3D-volume size=220mm(FH) 310mm(RL) 100mm(AP), MSDE Venc=1cm/s3, MSDE prep-time=50ms and scan duration=5m24s.
Results and Discussion
Fig.3(a) shows the compassion of MSDI delay time. A delay time of 200ms is found to be optimal for fat suppression over the full FOV. Fig.3(b) shows the comparison of the two types of MSDI refocusing pulses. A broadband adiabatic pulse improves the depiction of the nerves in the right side of brachial plexus. Fig.4 shows the representative images of MSDI-SHINKEI images by using optimal parameters. MSDI-SHINKEI clearly shows the brachial plexus structure with high SNR and uniform fat suppression.
Fig.5 shows the comparison of representative images and SNR among SPAIR-SHINKEI, STIR-SHINKEI and MSDI-SHINKEI. The fat suppression using MSDI is better than using SPAIR. The SNR of MSDI is significantly better than that of STIR. Furthermore, SNR of MSDI showed similar values compared to that of SPAIR. There was no significant difference. MSDI-SHINKEI thus retains the fat suppression homogeneity of STIR-SHINKEI, while maintaining the high SNR of SPAIR-SHINKEI.
Conclusion
MSDI could simultaneously suppress fat, flow and muscle signals using only one pre-pulse module. MSDI-SHINKEI provides uniform fat suppression in the brachial plexus, as in STIR, with no significant decrease in SNR compared to SPAIR. This sequence may be helpful to assess the nerve pathology in the brachial plexus.Acknowledgements
No acknowledgement found.References
1. Chhabra A, et al: High-Resolution 3T MR Neurography of the Brachial Plexus and Its Branches, with Emphasis on 3D Imaging. AJNR Am J Neuroradiol 2013;34:486–97
2. Vargas MI, et al. Three-dimensional MR imaging of the brachial plexus. Semin Musculoskelet Radiol. 2015;19:137-48.
3. Oudeman J, et al. Diffusion-prepared neurography of the brachial plexus with a large field-of-view at 3T. J Magn Reson Imaging. 2016;43:644-54.
4. Yoneyama M, et al. Rapid high resolution MR neurography with a diffusion-weighted pre-pulse. Magn Reson Med Sci. 2013;12:111-9.
5. Kasper JM, et al. SHINKEI--a novel 3D isotropic MR neurography technique: technical advantages over 3DIRTSE-based imaging. Eur Radiol. 2015;25:1672-7.
6. Madhuranthakam AJ, et al. Technical advancements in MR neurography. Semin Musculoskelet Radiol. 2015;19:86-93.
7. Wang J, et al. Enhanced image quality in black-blood mri using the improved motion-sensitized driven-equilibrium (iMSDE) sequence. J Magn Reson Imaging 2010;31:1256.
8. Obara M, et al. Comparison between two types of improved motion-sensitized driven-equilibrium (iMSDE) for intracranial black-blood imaging at 3.0 tesla. J Magn Reson Imaging. 2014;40:824-31.
9. Zwanenburg JJ, et al. MR Angiography of the cerebral perforating arteries with magnetization prepared anatomical reference at 7T: comparison with time-of-flight. J Magn Reson Imaging 2008;28:1519–1526.
Figures
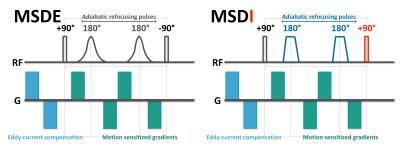
Fig.1. Differences of MSDE and MSDI pre-pulse.
MSDE is based on the improved MSDE (iMSDE), where additional eddy-current compensation is adopted in front of 90-degree pulse8. In MSDI the polarity of the final 90-degree pulse is inverted.
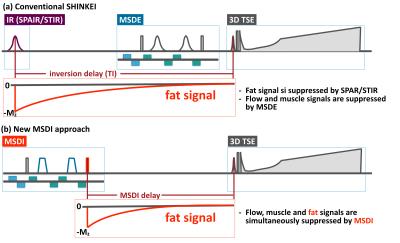
Fig.2. Methodological differences of conventional SHINKEI with IR-based fat suppression and MSDI prepared SHINKEI.
Conventional SHINKEI consists of both fat suppression IR (SPAIR or STIR) and MSDE preparation, with a 3D T2-weighted TSE sequence to acquire the data. The MSDE module has a long duration to suppress flow and muscle signal simultaneously. MSDI-prepared SHINKEI uses only one pre-pulse module, but this can suppress the fat tissues by inverting the fat signals due to the final 90-degree pulse. Consequently, MSDI enables the suppression of fat, flow and muscle signals simultaneously.
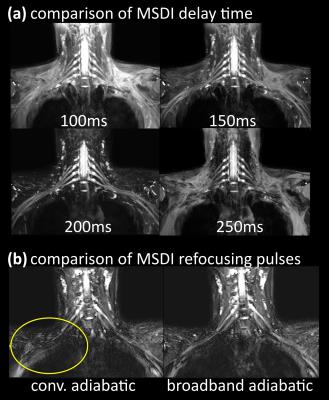
Fig.3(a). Compassion of MSDI delay-time. A delay time of 200ms is found to be optimal for fat suppression over the full FOV.
Fig.3(b). Comparison of two types of MSDI refocusing pulses. A broadband adiabatic pulse improves the depiction of the nerves in the right side of brachial plexus (yellow circle).
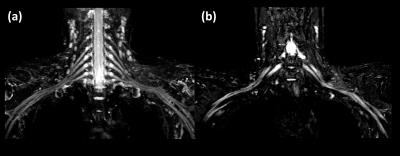
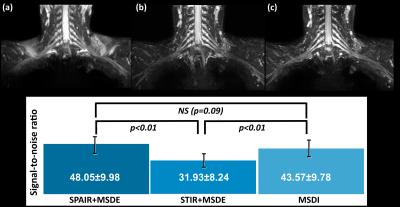
Fig.5. Comparison of representative images and SNR among SPAIR-SHINKEI (a), STIR-SHINKEI (b) and MSDI-SHINKEI (c).
The fat suppression using MSDI is better than using SPAIR. The SNR of MSDI is significantly better than that of STIR. Furthermore, SNR of MSDI showed similar values compared to that of SPAIR. There was no significant difference. MSDI-SHINKEI thus retains the fat suppression homogeneity of STIR-SHINKEI, while maintaining the high SNR of SPAIR-SHINKEI.