0832
LONGITUDINAL MONITORING OF DISEASE PROGRESSION IN CHILDREN WITH MILD CYSTIC FIBROSIS USING HYPERPOLARISED GAS MRI AND LUNG CLEARANCE INDEX1University of Sheffield, Sheffield, United Kingdom, 2Sheffield Children's Hospital, Sheffield, United Kingdom, 3Manchester Adult CF Centre, Manchester, United Kingdom
Synopsis
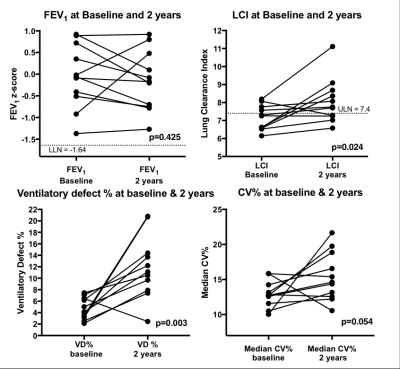
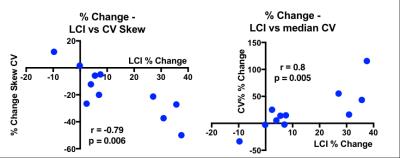
Hyperpolarised gas ventilation MRI is a sensitive method for evaluating disease progression in subjects with cystic fibrosis and normal spirometry. Ventilation defect % (VD%) increased in 10/11 subjects studied with a mean change of 201%. The MRI coefficience of variance (CV) of signal intensity was similarly sensitive to change. 10/11 subjects had increased lung clearance index (LCI) at 2-years but no subject had abnormal spirometry at either visit. The % change in LCI demonstrated strong correlations with the % change in CV outcomes. VD% and CV reflect different but complimentary aspects of lung disease that appear to track disease progression.
Introduction
Cystic fibrosis (CF) is a genetic condition with lung disease occurring progressively from birth and is the primary cause of early mortality. Accurate assessment of lung function in CF is key to maintaining lung health. Spirometry and the forced expiratory volume in 1 second (FEV1) is recognised as the primary lung function outcome in CF, yet FEV1 is insensitive to early and small changes in lung disease but remains the clinical standard. Hyperpolarised gas ventilation MRI (HP-MRI) allows direct visualisation of lung ventilation after the inhalation of a hyperpolarised noble gas. In mild CF, small ventilation defects are often visible using HP-MRI, which has been shown to be more sensitive than FEV1, CT and the lung clearance index (LCI) at detecting early lung disease(1). In this work we investigate whether HP-MRI would be able to effectively monitor CF disease progression with time, and whether ventilation MRI metrics would be more sensitive to longitudinal change than LCI or spirometry.Methods
11 children with CF and an FEV1 in the normal range (>-1.64 z-score) were assessed at baseline and 2 years later. At each visit subjects performed HP-MRI, spirometry and LCI. HP-MRI was performed on a 1.5T GE HDx scanner, hyperpolarised 3He was inhaled from functional residual capacity from a 1L Tedlar® bag partially filled with equal amounts of HP-3He and N2. The volume of 3He was titrated based on the height of the child and their lung volume at FRC. 2D SPGR ventilation images were acquired at a resolution of 3x3x10mm(2). Each ventilation image was registered to a segmented 1H structural image acquired during the same breath hold. The images were then assessed for the ventilated defect volume (VD%), calculated as the percentage of the lung volume without ventilation. Additionally, co-efficient of variance maps for the signal intensity acquired in each voxel across the ventilated lung (CV%) - a marker of ventilation heterogeneity. CV% was calculated by down-sampling each 2D DICOM image to 128x128 matrix. Lung volume masks derived from the proton image segmentation were eroded by one pixel to avoid region of partial volume effects. CV% maps were created using a 3x3 window centered on each voxel within the binary mask corresponding to the ventilated region. CV histograms were created and the median and skew reported. Spirometry was performed according to international guidelines(3). LCI was performed on a modified open-circuit Innocor utilising 0.2% SF6 as the tracer gas for wash-out(4).Results
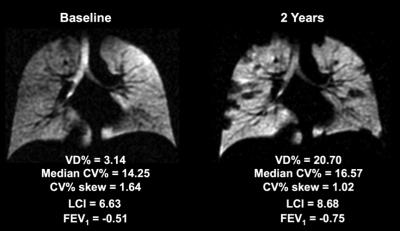
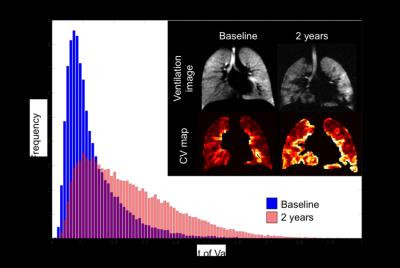
Results expressed as mean (sd) of all subjects. All subjects had ventilation defects evident on ventilation MRI at baseline, which significantly worsened at 2 years in 10/11 subjects (Figure 1). VD% was significantly increased from baseline to 2 years (4.69 (1.86) vs 11.89 (5.47)%, p=0.003). Median CV% was increased in 8/11 subjects at 2 years compared to baseline, though the difference was not statistically significant (12.92 (1.87) vs 15.43 (3.46)%, p=0.054). CV% skew significantly decreased in 10/11 subjects (1.62 (0.19) vs 1.31 (0.19), p=0.01). FEV1 did not change significantly over 2 years: baseline FEV1 z-score = -0.05 (0.74) vs -0.15 (0.69), at 2 years (p=0.425). 4/11 subjects had an abnormal LCI at baseline. At 2 years, LCI had increased significantly in 10/11 subjects with 7/10 subjects showing abnormal LCI: baseline 7.15 (0.69) vs 2 years 8.08 (1.25), p=0.024. Only 1 subject demonstrated improved lung function at 2 years, with a decreased VD% and median CV%, an increased CV% skew and a decreased LCI. In all subjects, VD% showed the largest mean change of 201%, whereas the mean change in LCI =13.5%, median CV% =22.9% and CV% skew =-17.4%. The % change in LCI correlated significantly with the % change of both median CV% (r=0.8, p=0.005) and CV% skew (r=-0.79, p=0.006) (Figure 2) but not with % change in VD%. Figures 3 and 4 demonstrate ventilation images and CV histograms respectively in CF subjects between visits.Discussion
Our results suggest that in these subjects with CF and sub-clinical lung disease, VD% from HP ventilation MRI is a sensitive metric of change in lung function that occurred in parallel with LCI change, however VD% demonstrated a much greater % change. Markers of CV% were similarly sensitive to longitudinal changes in lung function, and when combined with VD% describe different but complimentary pathophysiology. The strong correlations between % change in CV metrics and LCI suggest that the measurements are likely probing similar pathophysiology.Conclusion
Hyperpolarised gas ventilation MRI is capable of detecting sub-clinical lung disease in well children with CF. In addition, HP-MRI shows enhanced sensitivity for detecting longitudinal lung function deterioration than both LCI and FEV1.Acknowledgements
No acknowledgement found.References
1. Marshall H, Hughes D, Horsley A, Horn F, Smith L, Parra-Robles J, et al. Detection of early-stage lung disease in cystic fibrosis; comparing the sensitivity of 3He and 1H MRI, CT and LCI. European Respiratory Journal. 2014;44(Suppl 58).
2. Horn FC, Deppe MH, Marshall H, Parra-Robles J, Wild JM. Quantification of regional fractional ventilation in human subjects by measurement of hyperpolarized 3He washout with 2D and 3D MRI. Journal of applied physiology (Bethesda, Md : 1985). 2014;116(2):129-39.
3. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. European Respiratory Journal. 2005;26(2):319-38.
4. Horsley AR, Gustafsson PM, Macleod KA, Saunders C, Greening AP, Porteous DJ, et al. Lung clearance index is a sensitive, repeatable and practical measure of airways disease in adults with cystic fibrosis. Thorax. 2008;63(2):135-40.
Figures