0827
Functional lung MRI using matrix pencil decomposition and N2 multiple-breath washout measurements in cystic fibrosis1Division of Radiological Physics, Department of Radiology, University of Basel Hospital, Basel, Switzerland, 2Department of Biomedical Engineering, University of Basel, Basel, Switzerland, 3Division of Respiratory Medicine, Department of Pediatrics, University Children's Hospital of Bern, Bern, Switzerland, 4Department of Pediatric Pneumology, University Children's Hospital Basel (UKBB), Basel, Switzerland, 5University Institute for Diagnostic, Interventional and Pediatric Radiology, Inselspital, Bern University Hospital, Bern, Switzerland, 6Department of Radiology, University of Basel Hospital, Basel, Switzerland
Synopsis
This study examines a correlation between the functional lung MRI using matrix pencil decomposition and lung function tests in patients with cystic fibrosis. A strong correlation between the global ventilation inhomogeneity index (LCI) from multiple breath washout and ventilation/perfusion impairment in the lung determined by functional MRI is observed. The results of our study support the potential of functional MRI as a diagnostic tool in monitoring disease progression in cystic fibrosis.
Purpose
Cystic fibrosis (CF) is the most common severe autosomal recessive genetic disease in Caucasians that particularly affects the respiratory system. The genetic mutation in CF causes abnormal production and composition of airway surface fluid, which leads to chronic lung infections, airway obstruction, and alteration of pulmonary perfusion and ventilation.1
In this study, we performed examinations in CF patients using N2 multiple-breath washout (N2-MBW)2 and pulmonary functional matrix pencil decomposition MRI3 a derivative of Fourier decomposition MRI4, to compare the information obtained from each modality.
Methods
Forty pediatric patients with CF (mean age=11.6y, 25 females, 15 males) were enrolled into the study. Patients underwent MRI and N2-MBW on the same day. The study was approved by local Ethics Committee.
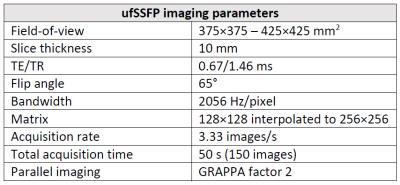
MRI was performed on a 1.5T clinical scanner in free-breathing without the administration of contrast agent. Lung function was studied using matrix pencil (MP) decomposition technique based on ultra-fast steady-state free precession imaging5 (Table 1). MP decomposition yielded fractional ventilation (FV) which reflects lung parenchyma density changes during respiration, as well as the perfusion (Q) and pulmonary blood arrival time.3 MR examinations were performed without sedation. Lung regions were semi-automatically segmented using a region growing algorithm. The signal distributions on the segmented ventilation and perfusion images were analyzed to estimate threshold values indicating functional impairment equal to 0.75 of median value from voxel distributions.6 Eventually, values of relative impaired ventilation (RFV) and perfusion (RQ) were calculated.
N2-MBW was performed using ExhalyzerD (EcoMedics, Switzerland) which yielded the lung clearing index (LCI), a main outcome parameter for global ventilation inhomogeneities.
Results
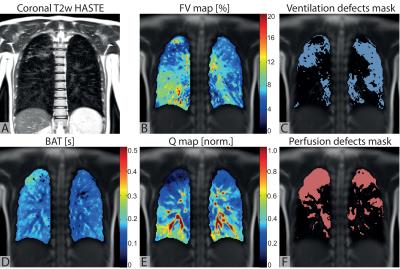
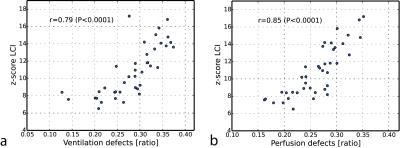
Exemplary functional and structural coronal chest images obtained in a CF patient are shown in Figure 1. The functional maps are characterized by inhomogeneous distribution of ventilation, perfusion and regions with delayed blood arrival time. Regions with reduced pulmonary function were automatically detected. The relative impairment of ventilation (RFV) ranged from 19% to 38% and the relative impairment of perfusion (RQ) ranged from 16% to 35%. Strong and statistically significant correlations were found between RFV and LCI (r=0.79,P<10-4) as well as RQ and LCI (r=0.85,P<10-5) (Figure 2).
Discussion and Conclusion
The results of our study support the role for functional MRI as a diagnostic tool in monitoring disease progression in patients with cystic fibrosis. Functional MR examinations using the matrix decomposition technique are easy to perform on a standard clinical MR scanner and require only minimal patient compliance.
Ventilation and perfusion impairment in the lung derived from MP MRI correlated strongly with the LCI, and thus seems promising as an quantitative outcome measure for diagnostic monitoring or as an end point for randomized control trials.
Acknowledgements
Swiss National Science Foundation; Grant number: SNF 320030_149576.References
1. Gibson RL, Burns JL, Ramsey BW. Pathophysiology and management of pulmonary infections in cystic fibrosis. Am J Respir Crit Care Med. 2003 Oct15;168(8):918-51.
2. Subbarao P, Milla C, Aurora P et al. Multiple-Breath Washout as a Lung Function Test in Cystic Fibrosis. A Cystic Fibrosis Foundation Workshop Report. Ann Am Thorac Soc. 2015 Jun;12(6):932-9.
3. Bauman G, Bieri O. Matrix pencil decomposition of time-resolved proton MRI for robust and improved assessment of pulmonary ventilation and perfusion. Magn Reson Med. 2016 Jan 12. doi: 10.1002/mrm.26096.
4. Bauman G, Puderbach M, Deimling M et al. Non-contrast-enhanced perfusion and ventilation assessment of the human lung by means of fourier decomposition in proton MRI. Magn Reson Med. 2009 Sep;62(3):656-64.
5. Bieri O. Ultra-fast steady state free precession and its application to in vivo (1)H morphological and functional lung imaging at 1.5 tesla. Magn Reson Med. 2013 Sep;70(3):657-63.
6. Bauman G, Puderbach M, Heimann T et al. Validation of Fourier decomposition MRI with dynamic contrast-enhanced MRI using visual and automated scoring of pulmonary perfusion in young cystic fibrosis patients. Eur J Radiol. 2013 Dec;82(12):2371-7.
Figures