0805
Robust MR Lymphangiography using DARC-MRL: Evaluation of Venous Suppression and Strategies for More Efficient Clinical Examinations1Radiology, University of Washington, Seattle, WA, United States, 2Diagnostic Services, Puget Sound VA HCS, Seattle, WA, United States, 3Plastic Surgery, University of Washington, Seattle, WA, United States
Synopsis
Dual Agent Relaxation Contrast MR Lymphangiography (DARC-MRL) effectively eliminates venous enhancement through the up-front i.v. injection ferumoxytol (USPIO causing marked blood T2* shortening) combined with obtaining MRL datasets at prolonged, precisely determined echo times. Echo time prolongation does cause an approximately 45% loss of lymphatic signal intensity, however with excellent lymphatic-to-tissue contrast, there was no clinically significant lymphatic signal loss. Data regarding the time course of lymphatic enhancement progression demonstrate most MRL enhancement can be fully captured in only two time points, allowing for a more efficient, faster examination. Multi-echo DARC offers to add further robustness and visualization capability.
Background
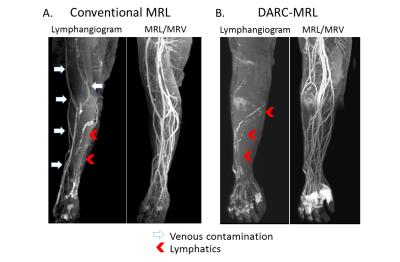
Lymphedema is a debilitating disease, with an estimated 10 million US individuals affected (90 million worldwide), primarily related to breast or pelvic cancer treatment.[1] Dual Agent Relaxivity Contrast MR Lymphangiography (DARC-MRL) has been recently introduced as a high-resolution technique for assessing lymphatics prior to therapeutic microsurgical lymphatico-venular anastomosis (LVA).[2] Similar to conventional MRL techniques, intracutaneous gadolinium-based contrast agent (GBCA) is injected into the hand or foot to opacify lymphatics. DARC-MRL, however, additionally administers i.v. ferumoxytol (USPIO; Feraheme, AMAG) to null unwanted venous signal resulting from GBCA uptake, a common issue that often complicates lymphatic visualization. Venous nulling is achieved by appropriate echo time (TE) elongation combined with the dramatic intravascular T2* shortening properties of ferumoxytol.
This study examines the utility of DARC-MRL in terms of venous enhancement (as compared to conventional MRL), lymphatic signal loss secondary to lymphatic T2* effects at the longer TE’s used for DARC, and the time course of lymphatic progression. Additionally, a multi-echo (mDARC) technique is introduced, simplifying the determination of the proper TE for venous nulling and allowing for added visualization possibilities.
Methods
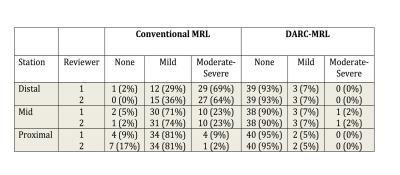
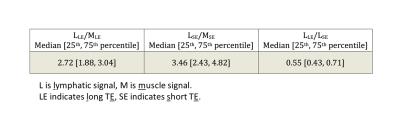
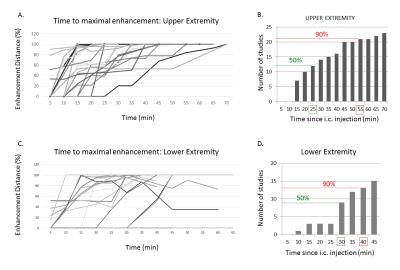
This IRB approved retrospective study identified 42 patients who underwent DARC-MRL (27 upper, 15 lower extremity) and 42 matched controls who underwent conventional MRL. Patients were imaged at 3T (Ingenia, Philips) using a two point mDixon technique [3] (approximate resolution 1.3 x 1.3 x 1.6 mm3 upper, 1.5 x 1.5 x 2.0 mm3 lower extremities, reconstructed as water-only images). Lymphatic opacification was achieved by intracutaneous administration of 1 ml GBCA (gadobenate dimeglumine, Bracco) into each webspace (hand or foot). For DARC-MRL, ferumoxytol 5 mg/kg was administered intravenously prior to intracutaneous GBCA to facilitate nulling of any venous contamination. In each DARC-MRL patient, the shortest TE pair required for blood pool suppression was determined through a set of “TE Scout” images. 3D mDixon datasets were then acquired over 30-90 min to follow the transit of GBCA through the lymphatics. The time course of progression (relative to maximum visualized lymphatic extent) was mapped. At the conclusion (most studies), a venogram was obtained: for conventional MRL, single dose GBCA was injected intravenously and venous phase images obtained; and for DARC-MRL, shortest TE (1.4/2.5 ms) mDixon was performed to create a dual MRL/MR venogram (MRL/MRV). Studies were divided into 3 zones (proximal, mid, distal) and subjectively graded (2 radiologists) for degree of venous contamination and any lymphatic signal loss with DARC (compared to MRL/MRV). DARC lymphatic and muscle signal intensity (SI) was measured and normalized (based on expected muscle SI loss) to determine the degree of lymphatic SI loss attributable to the longer DARC TE. Additional acquisitions (separate, IRB-approved study patients, n=9) were performed using a prototype mDARC sequence able to reconstruct perfectly registered mDixon images at 5 different TE pairs (acquired TEn ≈ 1.5 + 1.2n, n = 1-6).Results
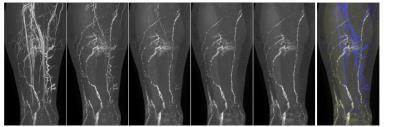
Venous contamination occurred in 41 of 42 conventional MRL (98%), but only 5-10% DARC-MRL studies (Figure 1, Table 1). Furthermore, contamination was rated as “problematic” in distinguishing lymphatics from veins in 64-69% of conventional MRL, but only one case (2%) of DARC-MRL. After normalization (considering appropriate muscle T1, T2*), DARC lymphatic signal loss was 45%, representing T2* effects coupled with the echo time elongation (Table 2). Subjectively, 35% and 48% of DARC exams (reviewers 1 and 2) were scored as no loss of lymphatic signal at long TE. The remaining exams (65% and 52%) were scored as patchy loss of signal, not felt to be clinically significant. The maximal extent of lymphatic opacification was achieved in 50% of studies by 25 minutes, and 90% by 55 minutes in upper extremity; and 50% by 30 minutes and 90% by 40 minutes in lower extremities (Figure 2). Figure 3 demonstrates 5 progressively lengthened echo datasets from mDARC.Discussion
DARC-MRL essentially eliminates confounding venous enhancement. Furthermore, despite an approximate 45% lymphatic SI loss at the DARC longer echo times, excellent lymphatic-to-soft tissue contrast is seen without obvious clinical detriment. Based on the lymphatic progression timing data, we were able to modify our DARC-MRL protocol such that a) patient injected with feraheme outside magnet, b) i.c. GBCA injection occurs on magnet immediately prior to initiating imaging, and c) MRL datasets are only obtained at approximately 25 and 50 minutes. This considerably shortens the MRL exam. A new refinement, mDARC promises to add further robustness and speed by eliminating the time and potential error of proper TE choice, eliminating the need for a separate MRL/MRV acquisition, and adding interesting post-processing possibilities given multiple registered datasets with differing relative lymphatic and vascular signal intensities.Acknowledgements
This work was in part funded by a grants from the Safeway Foundation and Philips Healthcare.References
1. Szuba A, Shin WS, Strauss HW, Rockson S. The third circulation: radio-nuclide lymphoscintigraphy in the evaluation of lymphedema. J Nucl Med 2003;44:43–57.
2. Maki JH, Neligan PC, Briller N, Mitsumori LM, Wilson GJ. Dark Blood Magnetic Resonance Lymphangiography Using Dual-Agent Relaxivity Contrast (DARC-MRL): A Novel Method Combining Gadolinium and Iron Contrast Agents. Curr Probl Diagn Radiol 2016;45:174-179.
3. Eggers H, Brendel B, Duijndam A, Herigault G. Dual-echo Dixon imaging with flexible choice of echo times. Magn Reson Med 2011;65:96-107.
Figures