0799
Assessment of Carotid Atherosclerotic Disease Using 3D Simultaneous Non-contrast Angiography and Intraplaque Hemorrhage (SNAP) imaging: Comparison with Digital Subtraction Angiography1Radiology, Renji Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, People's Republic of China, 2MR Clinical Science, Philips Healthcare, Greater China, People's Republic of China, 3University of Washington, WA, United States, 4Center for Biomedical Imaging Research,Department of Biomedical Engineering, Tsinghua University, Beijing, People's Republic of China
Synopsis
3D fast Simultaneous Non-contrast Angiography and intraPlaque hemorrhage (SNAP) imaging was recently proposed as a technique for joint MRA and intraplaque hemorrhage (IPH) imaging. This study sought to determine the accuracy of this technique at quantifying carotid atherosclerosis disease compared to conventional intra-arterial digital subtraction angiography (DSA) in patients with at least 50% carotid stenosis. We found that 3D SNAP imaging had excellent agreement with DSA in measuring luminal stenosis and identification of ulceration in carotid arteries. Our findings suggest that, SNAP imaging might be a potential candidate technique for comprehensive evaluation of carotid high-risk atherosclerotic disease.
Introduction
Both luminal stenosis and vulnerable plaque features, such as intraplaque hemorrhage (IPH) and fibrous cap rupture or unlceration, have been considered as key imaging biomarkers for high-risk atherosclerotic disease[1,2]. Recently, 3D fast Simultaneous Non-contrast Angiography and intraPlaque hemorrhage (SNAP) imaging was proposed for joint MRA and IPH imaging[3]. Wang et al compared SNAP MRA with Time-of-Flight (TOF) technique in measuring carotid artery lumen area[3]. However, clinically, catheter angiography is the gold standard in evaluating luminal stenosis of carotid arteries. As such, validation of SNAP imaging by digital subtraction angiography (DSA) is warranted. The purpose of this study was to determine the accuracy of 3D SNAP imaging in characterizing carotid atherosclerotic disease compared to DSA.Methods
Study sample: Symptomatic patients with ≥50% stenosis in unilateral carotid artery identified by duplex ultrasound were recruited and underwent 3D SNAP MR imaging and DSA within 1 week. Conventional intra-arterial DSA studies were performed using a trans-femoral artery approach and selective common carotid artery catheterization on a digital angiography unit. MR imaging: SNAP imaging was performed on a 3.0T whole-body MR scanner (Philips, Achieva TX) with a dedicated 8-channel phased-array carotid coil. The SNAP sequence was acquired with the following parameters: phase sensitive inversion recovery enabled 3D inversion recovery turbo field echo, TR/TE 10/4.8 ms, flip angle 11°, field of view 160×32×160mm3, spatial resolution 0.8×0.8×0.8mm3, and scan time 2min 17sec. Data analysis: Carotid SNAP and DSA images were independently reviewed by two experienced radiologists with consensus. The image quality (IQ) of SNAP images was assessed. The SNAP images were first processed for MRA and IPH visualization as described before[3]. The degree of stenosis according to the NASCET criteria was measured and the presence/absence of plaque ulceration was determined by SNAP and DSA imaging separately and compared between these two imaging techniques.Results
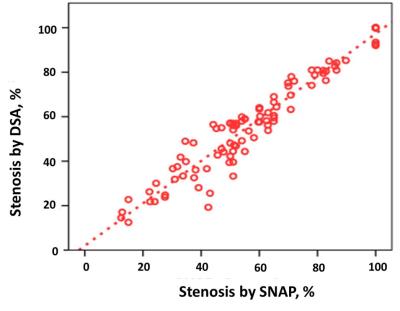
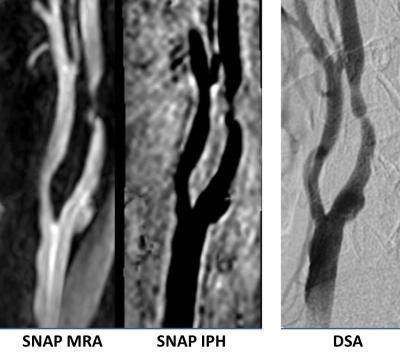
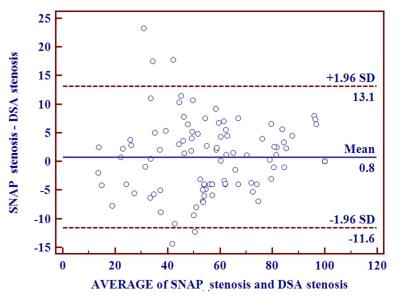
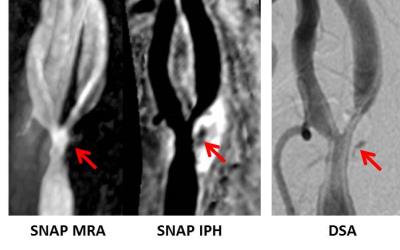
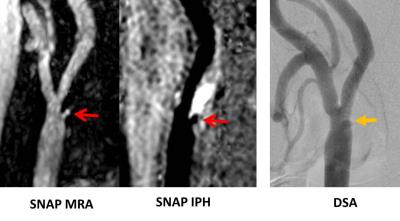
In total, 55 patients (mean age 64.9 years, 42 males) were included in the final statistical analysis. SNAP images from 9 of 110 (8.2%) carotid arteries were excluded from analysis due to either inadequate IQ (n=7) or excessive vascular tortuousness at the site of greatest narrowing (n=2). Of the remained 101 arteries, excellent agreement in measuring luminal stenosis was found between 3D SNAP imaging and DSA (intraclass confidence interval: 0.978; 95% CI: 0.968-0.985) (Fig.1, 2). Bland-Altman plots showed that the bias between 3D SNAP imaging and DSA differed before and after 80% stenosis (Fig.3). On DSA, 13 arteries were found to have ulcerations. The 3D SNAP imaging was also found to have high sensitivity (91.7%), specificity (96.2%) and excellent agreement (Cohen’s κ=0.86; 95% CI: 0.68-0.99) with DSA in identification of ulceration (Fig. 4).Discussion and conclusions
This study investigated the performance of 3D SNAP imaging in assess carotid artery luminal stenosis and ulceration compared with DSA. We found that 3D SNAP imaging had excellent agreement with DSA in measuring luminal stenosis and identification of ulceration in carotid arteries. In the present study, post-hoc analysis after inspecting the Bland-Altman plots suggested that the bias between 3D SNAP imaging tended to slightly over-estimate when DSA stenosis was >80%. Multiple factors may contribute to the stenosis measurement bias, including spatial resolution, sequence type and postprocessing algorithms. Although we carefully researched and minimized potential sources of bias before making our measurements, the discrepancy of viewing angles of the carotid lesions would inevitably hamper the agreement analysis. Repeated re-slicing of the 3D image data with multiple views may be helpful for assessment of stenosis and ulceration(Fig. 5). With its fast acquisition and large coverage, SNAP imaging might be a potential candidate technique for comprehensive evaluation of carotid high-risk atherosclerotic disease.Acknowledgements
None.References
1. Saam T, Underhill HR, Chu B, et al. Prevalence of american heart association type VI carotid atherosclerotic lesions identified by magnetic resonance imaging for different levels of stenosis as measured by duplex ultrasound. J Am Coll Cardiol. 2008;51:1014-1021
2. Finn AV, Nakano M, Narula J, et al. Concept of vulnerable/unstable plaque. Arterioscler Thromb Vasc Biol .2010;30:1282-1292.
3. Wang J, Börnert P, Zhao H, et al. Simultaneous noncontrast angiography and intraplaque hemorrhage (SNAP) imaging for carotid atherosclerotic disease evaluation. Magn Reson Med. 2013; 69(2):337-345.
Figures