0797
Coronary Plaque Hyper-Intensity on Dark-Blood T1-Weighted MRI Helps Identify Lesion-Specific Ischemia: Insights from the Comparison Study with Invasive Fractional Flow Reserve (FFR)1Biomedical Imaging Research Institute, Cedars-Sinai Medical Center, Los Angeles, CA, United States, 2Department of Radiology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea, Republic of, 3Division of Cardiology, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea, Republic of, 4Siemens Healthcare, Chicago, IL, United States, 5Heart Institute, Cedars-Sinai Medical Center, Los Angeles, CA, United States
Synopsis
Coronary Atherosclerosis T1-weighted Characterization (CATCH) is an accelerated MR technique for detecting high-risk atherosclerotic lesions. However, the relationship between plaque signal and lesion-specific ischemia is still unclear. In this
Purpose
Fractional Flow Reserve (FFR) measurement is the current gold standard for identifying coronary lesions that cause ischemia1. This technique, albeit costly and invasive, provides valuable input for guiding treatment decisions, particularly for lesions with intermediate level of stenosis2. Although coronary hyper-intensive plaques (CHIPs) on dark-blood T1-weighted MRI are associated with future major events3, their relationship with lesion-specific ischemia remains unclear. We recently developed an improved acquisition scheme, Coronary Atherosclerosis T1-weighted Characterization (CATCH), providing integrated anatomical reference, shortened scan time, improved spatial resolution and whole-heart coverage4. This study utilized CATCH to evaluate the association between CHIPs and lesion-specific ischemia by FFR.Methods
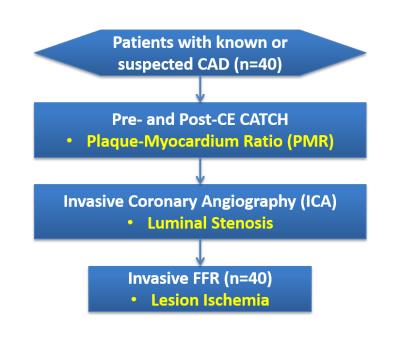
Using the previously published CATCH protocol4, we studied 40 consecutive patients (28 men and 12 women, mean age: 61±9) with new-onset or recurrent stable angina for whom coronary catheterization was planned (Figure 1). After receiving CATCH scans pre- and post-contrast enhancement, patients underwent invasive coronary angiography (ICA) and FFR measurements. Pre- and post-contrast Plaque-to-Myocardial Ratio (PMR) was quantified in 55 lesions blinded to invasive imaging results and compared with location-matched FFR data. PMR was dichotomized using the receiver-operating characteristics (ROC) analysis to determine the optimal thresholds for discrimination of ischemia (FFR ≤0.80). Incremental discrimination of ischemia by PMR was evaluated by area under the curve (AUC) analysis of the receiver operating characteristic (ROC). Logistic regression analysis was employed to evaluate the predictors of ischemia.Results
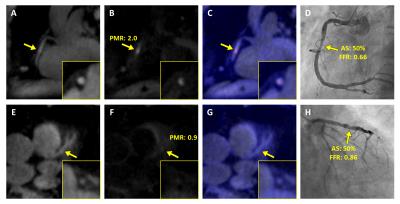
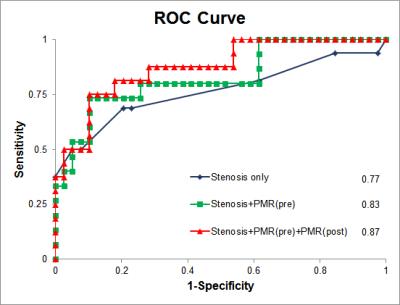
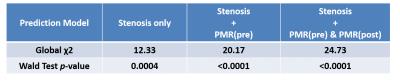
Figure 2 shows two representative patient study cases in comparison. With the identical level of intermediate luminal stenosis (50%), the hyper-intensive lesion (PMR=2.0) was causal of ischemia (FFR=0.66), whereas the hypo-intensive lesion (PMR=0.9) was not hemodynamically significant (FFR=0.86). Figure 3 presents the global ROC analysis showing increased AUC with the inclusion of pre- and post-contrast PMR compared with stenosis along. Table 1 summarizes the logistic regression statistics showing increased predictive ability provided by adding PMR for the detection of lesion-specific ischemia.Discussion
The exact pathophysiological mechanism behind the observed link between MR plaque hyperintensity and lesion-specific ischemia is currently not clear. We hypothesize that this relationship is bridged by abnormal arterial wall shear stress resulting from hemodynamic changes, which is known to alter the endothelial functions and lead to plaque progression5. The results presented here suggested that MR coronary plaque imaging may provide added value for assessing the “treatment-worthiness” of individual lesions. Because MR plaque imaging is noninvasive and does not involve ionizing radiation, it has the potential to serve as a “gate-keeper” for invasive and costly coronary exams or more aggressive interventions.Conclusion
The comparison study between CATCH and invasive FFR suggested that coronary plaque hyper-intensity on dark-blood T1-weighted MRI provides independent improvement for the identification of ischemia-causing lesions compared with stenosis evaluation alone. Further study with a larger sample size is warranted and currently underway.Acknowledgements
Grant Support: NHLBI
R01 HL096119 and NRF 2012027176.
References
1 Tonino, P. A. et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. The New England journal of medicine 360, 213-224, doi:10.1056/NEJMoa0807611 (2009).
2 Pijls, N. H. et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. Journal of the American College of Cardiology 49, 2105-2111, doi:10.1016/j.jacc.2007.01.087 (2007).
3 Noguchi, T. et al. High-Intensity Signals in Coronary Plaques on Noncontrast T1-Weighted Magnetic Resonance Imaging as a Novel Determinant of Coronary Events. Journal of the American College of Cardiology 63, 989-999, doi:10.1016/j.jacc.2013.11.034 (2014).
4 Xie, Y. et al. Coronary Atherosclerosis T1-Weighed Characterization With Integrated Anatomical Reference: Comparison With High-Risk Plaque Features Detected by Invasive Coronary Imaging. JACC. Cardiovascular imaging, doi:10.1016/j.jcmg.2016.06.014 (2016).
5 Samady, H. et al. Coronary artery wall shear stress is associated with progression and transformation of atherosclerotic plaque and arterial remodeling in patients with coronary artery disease. Circulation 124, 779-788, doi:10.1161/CIRCULATIONAHA.111.021824 (2011).
Figures