0743
Passive Tracking Sequence with Positive Contrast using Partial Saturation for MR-guided Cardiac CatheterisationMari Nieves Velasco Forte1, Kuberan Pushparajah1, Nycholas Byrne2, Mazen Alhrishy1, Bram Ruijsink1, Israel Valverde1,3, Tobias Schaeffter1, Reza Razavi1, and Sébastien Roujol1
1Division of Imaging Sciences & Biomedical Engineering, King's College London, London, United Kingdom, 2Medical Physics, King's College London, London, United Kingdom, 3Cardiovascular Imaging, Institute of Biomedicine of Seville, Seville, Spain
Synopsis
Cardiac MRI-guided catheterization offers an alternative to conventional fluoroscopy. This technique has been used in congenital heart disease for diagnostic purposes using passive tracking methods, with either CO2 or gadolinium filled balloon wedge catheters. The gadolinium filled balloon is easier to visualize. The sequence, real-time bSSFP, can be used with or without saturation prepulse, leading to either suppression of soft tissue signal or poor catheter visualization. We have developed a partial saturation pulse sequence providing high contrast between tissue, blood and balloon. After optimization in phantoms and volunteers, this sequence has shown excellent results during MR-guided catheterization in patients.
Purpose
Cardiac catheterisation is a common diagnostic and interventional procedure in patients with congenital heart disease (CHD). This procedure is commonly performed under X-ray guidance, associated with ionizing radiation and increased risks for cancer[1]. MRI-guided cardiac catheterization has been proposed to provide better soft tissue contrast, avoid ionizing radiation. Current passive catheter tracking approaches employ positive and negative contrast using gadolinium or CO2 filled balloon wedge catheters[2-4], respectively. Visualization of the Gadolinium filled balloon appears to be easier compared to the CO2-filled balloon[5]. However, gadolinium-filled balloon methods rely on real-time bSSFP images acquired without saturation (non-SAT) prepulse, which leads to poor catheter balloon/blood contrast or with saturation (SAT) prepulse which suppresses soft tissue/blood signal[5]. In this study, we developed and optimized a novel gadolinium-filled balloon positive contrast sequence to provide simultaneous high contrast visualization of soft tissue, blood and catheter balloon using a partial saturation (pSAT) pre-pulse.Methods:
The proposed sequence uses a real-time single shot acquisition with bSSFP readout (TR/TE=2.6ms/1.3ms, flip angle=60°, FOV=370×370mm2, voxel size=2.2×2.5mm2, bandwidth=1190Hz, SENSE factor=2.5, partial Fourier=0.65, acquisition time=145ms, linear ordering). Each image was acquired immediately after a saturation pre-pulse with a reduced saturation angle to only achieve partial saturation. Optimization of the pSAT angle was first performed using Bloch equation simulations. Different levels of intra-voxel partial voluming of the balloon wedge catheter (Arrow®) where analyzed with the balloon at the tip filled in with 1% gadolinium (DotaremÒ). The entire setup was initially tested using a 3D printed heart phantom and optimized in volunteers. Two patients aged 12 and 39 years in whom an XMR was clinically indicated for pulmonary vascular resistance assessment were recruited. Underlying diagnosis were severe right pulmonary stenosis and atrioventricular septal defect (child and adult, respectively). In the adult patient, the pSAT sequence was initially run several times to study the influence of the pSAT angle. Catheter balloon/blood CNR, catheter balloon SNR, blood SNR, and overall subjective assessment (by a cardiologist blinded from the simulation findings) of contrast quality were measured in the last image of each acquisition. MR-guided catheterization was performed in both patients using the pSAT sequence with a 30° SAT angle. The sequence was run in interactive mode and the imaging plane location was modified in real time by the interventional cardiologist using a set of pre-programmed pedals inside the scanner room. 1% gadolinium (Dotarem®) was used to fill the balloon of the wedge catheter for positive contrast visualization.Results:
Numerical simulations showed a 20-40° pSAT angle provides a good compromise between high catheter balloon/blood contrast, high SNR and reduced sensitivity to intra-voxel partial voluming of the catheter balloon (Figure 2). The proposed pSAT approach also provides better contrast than conventional non-SAT sequences (pSAT angle=0°) and better SNR than SAT sequences (pSAT angle=90°). The proposed sequence with a 20-40° pSAT angle provided a good in-vivo compromise between catheter balloon/blood CNR and blood SNR (Figure 1). The balloon of the wedge catheter was clearly depicted during navigation in the phantom with the pSAT sequence (Figure 2). Quantitative and qualitative assessment of the pSAT acquisitions with different pSAT angles confirmed the optimality of a 30° pSAT angle (Figure 3). In both patients the catheter was inserted via the femoral vein and directed through the inferior vena cava to the right atrium, right ventricle, pulmonary artery and its branches (Figure 4). The pSAT sequence was found successful to passively track the catheter and simultaneously visualize soft tissue and blood. However, in the first patient, the catheter lacked the stiffness required to cross the pulmonary valve. In this patient, the procedure was completed with X-ray support using a braided non-MRI compatible catheter over a wire with higher stiffness. The procedure was completed solely under MRI guidance in the second patient. Total procedure time was 172 and 170 minutes, cardiac catheterisation time was 55 and 25 min in child and adult, respectivelyDiscussion:
The proposed pSAT sequence provides real-time simultaneous high contrast visualization of the balloon wedge catheter, soft tissues and blood. This technique provides superior contrast than conventional non-SAT sequences and simultaneous visualization of soft tissues with excellent passive tracking capabilities during MR-guided catheterization in patients with congenital heart disease. This method uses modified commercially available sequences and could provide an alternative to catheterization in centers in which cardiac MRI is established as an imaging diagnostic tool.Conclusions:
In this preliminary experience, the described pSAT sequence offered real-time MR-guided passive tracking of catheters, with simultaneous high contrast visualization of human blood, soft tissue and the balloon of the wedge catheter.Acknowledgements
No acknowledgement found.References
1. Modan B, Keinan L, Blumstein T, Sadetzki S (2000) Cancer following cardiac catheterization in childhood. Int J Epidemiol 29 (3):424-428 2. Razavi R, Hill DL, Keevil SF, Miquel ME, Muthurangu V, Hegde S, Rhode K, Barnett M, van Vaals J, Hawkes DJ, Baker E (2003) Cardiac catheterisation guided by MRI in children and adults with congenital heart disease. Lancet 362 (9399):1877-1882. 3. Pushparajah K, Tzifa A, Razavi R (2014) Cardiac MRI catheterization: A 10-year single institution experience and review. Interventional Cardiology (London) 6 (3):335-346. 4. Pushparajah K, Tzifa A, Bell A, Wong JK, Hussain T, Valverde I, Bellsham-Revell HR, Greil G, Simpson JM, Schaeffter T, Razavi R (2015) Cardiovascular magnetic resonance catheterization derived pulmonary vascular resistance and medium-term outcomes in congenital heart disease. J Cardiovasc Magn Reson 17:28. 5. Ratnayaka K, Faranesh AZ, Hansen MS, Stine AM, Halabi M, Barbash IM, Schenke WH, Wright VJ, Grant LP, Kellman P, Kocaturk O, Lederman RJ (2013) Real-time MRI-guided right heart catheterization in adults using passive catheters. Eur Heart J 34 (5):380-389.Figures
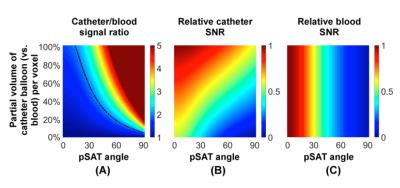
Signal simulation of
catheter balloon and blood using Bloch equations. Signal ratio between catheter
balloon and blood(A) and relative SNR of catheter balloon(B) and blood(C) in
function of the employed partial saturation (pSAT) angle and intra-voxel
partial volume of the catheter balloon (vs. blood). Dashed line (A) represents
a signal ratio of 2. Bloch equation simulations used a T1/T2 of 1500/250ms for
blood signal and 40/40ms for catheter balloon signal. A pSAT angle of 20-40°
provides a good compromise to ensure high catheter balloon/blood contrast, high
blood SNR and reduced sensitivity to partial volume of the catheter balloon.
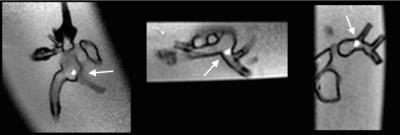
Example of real-time images acquired in the 3D printed
heart phantom with balloon wedge catheter using the pSAT sequence. The catheter
tip (arrows) could be easily tracked and visualized in different imaging plane
orientations.
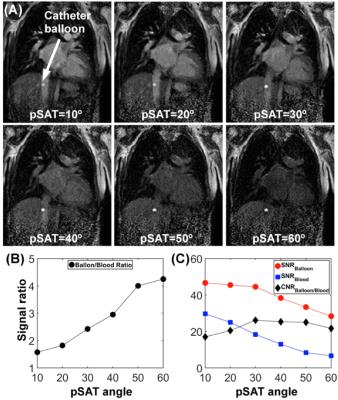
Real-time images
acquired using the pSAT sequence with different saturation angles in one
patient undergoing MR-guided catheterization (A). Signal ratio between catheter
balloon and blood (B). Signal-to-noise ratio (SNR) of catheter balloon and
blood, and contrast-to-noise ratio (CNR) between catheter balloon and blood are
shown in (C). High saturation angle leads to increased catheter balloon/blood
contrast and reduced SNR. A pSAT angle of 30° provided the higher balloon/blood
CNR and a good compromise between catheter balloon/blood signal ratio and blood
SNR drop. The image acquired with the 30° pSAT angle was also found as
providing the best subjective contrast quality.

Real-time acquired in the adult patient using the pSAT
sequence. Note balloon of the wedge catheter at the inferior vena cava (A),
main pulmonary artery (B) and left pulmonary wedge (C). The pSAT sequence
provided excellent and simultaneous visualization of catheter tip, blood and
soft tissues