0736
Real-Time MRI-Guided Targeted Needle Placement During Motion using Rolling-Diaphragm Hydrostatic Actuators1Radiological Sciences, University of California Los Angeles, Los Angeles, CA, United States, 2Biomedical Physics, University of California Los Angeles, Los Angeles, CA, United States, 3Mechanical and Aerospace Engineering, University of California Los Angeles, Los Angeles, CA, United States, 4Bioengineering, University of California Los Angeles, Los Angeles, CA, United States, 5Department of Radiology, Dongguk University Ilsan Hospital, Korea, Republic of
Synopsis
In this work, we present a new version of our hydrostatically actuated system and investigate its accuracy and time efficiency for real-time MRI-guided targeted needle placement in a motion phantom. We show that actuator-assisted needle placement was able to reach the targets with greater accuracy and in less time than free-hand step-and-shoot placement for both static and simulated respiration motion. Our new rolling-diaphragm hydrostatic actuators can potentially enable physicians to remotely perform real-time MRI-guided interventions during motion.
Introduction
Limited accessibility to the patient in bore has restricted the advancement of real-time MRI-guided interventions1. MR-compatible robotic systems are a potential solution to overcome this critical limitation. In particular, we have recently shown that hydrostatic actuation is inherently MR-compatible and can be used to create cost-effective systems2. In this work, we present a new version of our hydrostatically actuated system and investigate its accuracy and time efficiency for real-time MRI-guided targeted needle placement in a motion phantom.Methods
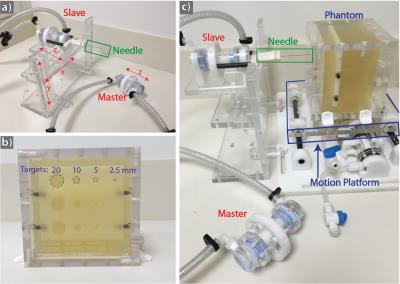
System Design: We designed new actuators using a rolling diaphragm2,3 to fully seal the hydrostatic cylinder. The diaphragms and actuator casing were all created in house. The system utilizes an identical master/slave actuator pair connected by closed fluid channels to transmit force and displacement into the bore (Fig. 1a).
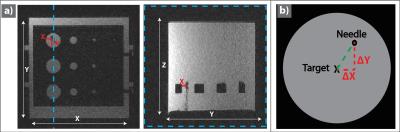
Phantom Design: In order to evaluate the accuracy of needle placement using the actuator system, a phantom containing a targeting plate with three rows of holes at different diameters (20, 10, 5, and 2.5 mm) was constructed (Fig. 1b). The phantom was filled with a dyed gelatin solution to obscure direct visualization (Fig. 2a).
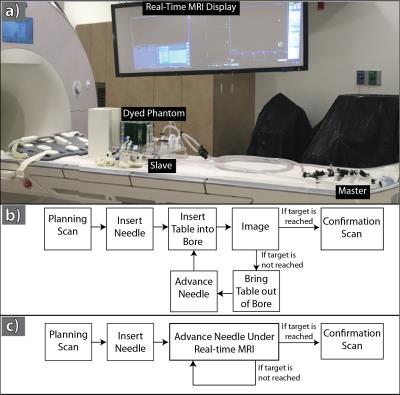
Experimental Design: The targeting phantom was secured onto an in-house manufactured motion platform and advanced into the scanner bore (Fig. 2). The operator was instructed to maneuver an MR-compatible biopsy needle (MReye, Cook Medical) to the center of each target and insert past the targeting plate. Once the operator believes the target was reached, a high resolution 3D GRE scan (TE/TR=1.82/4.1ms, FOV=300x300mm2, Resolution=1.1x1.1x2mm3, FA=10o) was acquired. All steps were timed (Fig. 2). This was performed with the motion phantom off (“static”) or with a sinusoidal waveform (“sinusoid motion”) of 0.3Hz and displacement range of 20mm (similar to a human respiratory cycle4,5) perpendicular to the needle (Fig 1) for the following strategies.
Step-and-shoot (SS): The operator moves the patient table and phantom out of the bore and uses planning images to insert the needle by hand into the target. The table is then returned to the bore and the phantom is imaged using a 2D GRE sequence. The phantom is then removed from the bore and using the images the needle is advanced further toward the target. This is repeated until the operator believes that the target is reached.
Actuator-Assisted (AA): The actuator system was adjusted along X-Y and the needle inserted into the phantom. The operator then manipulated the master actuator to control the slave actuator and guide the needle into the target under real-time 2D GRE.
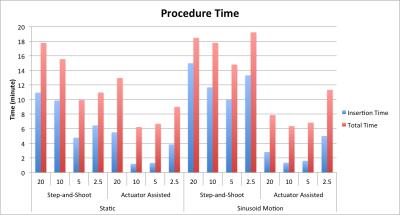
Targeting Analysis: For each experiment, insertion time (IT) (from initial insertion to when the target was reached) and total time (TT) (from the first planning scan to the final confirmation scan) were recorded. The X-Y Euclidean distance between the final needle tip position and the center of the target was measured to characterize targeting accuracy in terms of needle-to-target error (NTE) (Fig 3).
Results
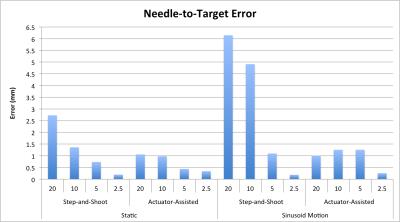
Targeting Accuracy: The NTE for each of the four targets was plotted (Fig. 4). The NTE for the two smaller targets (5 and 2.5 mm) were similar between the SS and AA methods for both motion states. For the larger targets, on average the AA method achieves 2.0 fold lower NTE than the SS method during static (NTESS = 2.0mm, NTEAA= 1.0mm) and 4.9 fold lower NTE during sinusoidal motion (NTESS = 5.5mm, NTEAA= 1.1mm).
Targeting Time: The insertion and total times for the four targets were plotted (Fig. 5). For the static case, on average the AA IT was 2.7 fold faster than the SS method (ITSS= 8.0, ITAA= 3.0 minutes), and the TT was 1.5 fold faster (TTSS= 13.6, TTAA = 8.7 minutes). For the sinusoidal motion case, on average the AA IT was on 4.6 fold faster than the SS method (ITSS= 12.5, ITAA= 2.7 minutes), and the TT was 2.2 fold faster (TTSS= 17.6, TTAA= 8.1 minutes).
Discussion and Conclusion
Our rolling-diaphragm hydrostatic actuator system was able to successfully guide the needle to all of the targets under real-time MRI guidance. Since the position of the target in bore was beyond reach, the operator could not perform real-time free-hand insertion. Clinically, physicians target lesions as small as 5 mm, which necessitates achieving NTE<2.5 mm - our initial results demonstrate feasibility for our actuator system to attain this accuracy, even under simulated respiratory motion. Also, longer procedure times increase complication risk for patients. The Actuator-Assisted method was able to reach the targets with greater accuracy and in less time than the Step-and-Shoot method. Our rolling-diaphragm hydrostatic actuator system can potentially enable physicians to remotely perform real-time MRI-guided interventions during motion.Acknowledgements
This project was supported in part by an NSF Graduate Research FellowshipReferences
1. Moche M, Zajonz D, Kahn T, Busse H. MRI-guided procedures in various regions of the body using a robotic assistance system in a closed-bore scanner: preliminary clinical experience and limitations. J. Magn. Reson. Imaging [Internet] 2010;31:964–74. doi: 10.1002/jmri.21990.
2. Mikaiel S, Simonelli J, Lu D, Sung K, Tsao T-C, Wu HH. Real-Time MRI-Guided Interventions using Rolling-Diaphragm Hydrostatic Actuators. In: ISMRM 24th Annual Meeting. ; 2016. p. 3588.
3. Whitney JP, Glisson MF, Brockmeyer EL, Hodgins JK. A Low-Friction Passive Fluid Transmission and Fluid-Tendon Soft Actuator. IEEE/RSJ Int. Conf. Intell. Robot. Syst. [Internet] 2014.
Figures