0714
Improved prediction of meningioma-brain adhesion with normalized octahedral shear strain using slip interface imaging based on MR-elastography1Radiology, Mayo Clinic, Rochester, MN, United States, 2Neurosurgery, Mayo Clinic, MN, United States, 3Physiology and Biomedical Engineering, Mayo Clinic, MN, United States, 4Naval Research Laboratory, Code 7160, Washington, DC
Synopsis
Knowledge of meningioma-brain adhesion can be important to surgical outcome but has been reliably assessed only during surgery. Slip interface imaging (SII), a recently developed MR-elastography based technique, is capable of determining the degree of meningioma-brain adhesion preoperatively. In SII, a non-adherent meningioma demonstrates a hyper-intense octahedral shear strain (OSS) contour along the tumor-brain interface. In 25 meningiomas, an algorithm improved by normalizing OSS to the combined wave amplitude provided a more accurate prediction in the setting of peritumoral edema. Normalized OSS increased SII accuracy from 72% to 92%, and the kappa coefficient increased from 0.37 (fair) to 0.86 (good).
Introduction
Knowledge of a meningioma’s attachment to adjacent normal tissue can be important to surgical outcome but has been reliably assessed only during the surgery. Recently, slip interface imaging (SII), a technique based on MR-elastography (MRE), has been developed to preoperatively evaluate tumor adherence at the tumor-brain interface noninvasively1,2. It has been shown that non-adherent vestibular schwannomas demonstrated higher octahedral shear strain (OSS) values along the tumor-brain interface than adherent tumors. However, the value of OSS is not only determined by the slip shear at the interface, but can also be influenced by the overall amplitude of the wave at the interface. In order to reduce these variations we developed a normalized OSS calculation in which the OSS is normalized to the wave amplitude. The goal of this study was to investigate the ability of OSS and normalized OSS to predict the degree of meningioma-brain adhesion.Methods
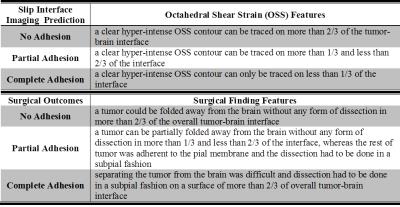
After institutional review board approval and written informed consent, 25 patients (mean age 61±11years) with a meningioma ≥2.5cm in maximum diameter were preoperatively assessed with MRE on 3T MR scanners. The SII technique is based on brain MRE1,3. Briefly, low amplitude mechanical vibrations at 60Hz were introduced intracranially with a soft pillow-like driver placed under the head. The resulting displacement field was imaged by a single-shot, flow-compensated, SE-EPI-MRE pulse sequence: TR/TE=3600/62ms, 3× parallel imaging acceleration, 48 axial slices with 3mm isotropic resolution, 8 phase offsets, and ±xyz 6 motion encoding directions. The scan time was under 7mins. OSS maps were calculated as previously described4. The phase data was unwrapped with an iterative 3D graph cuts based unwrapping algorithm5,6. The normalized OSS map was generated by normalizing OSS to the combined amplitude (square root of sum of squares) of the first harmonic of the complex xyz-axis shear waves. SII predictions and the neurosurgeon impression of tumor adhesion were graded on a 3-point scale: no adhesion, partial, and complete adhesion (Tab.1). The Cohen κ coefficient was used to study the agreement between the SII prediction and surgical findings. The correlation was assessed by using the Chi-square test (significance level <0.05).Results
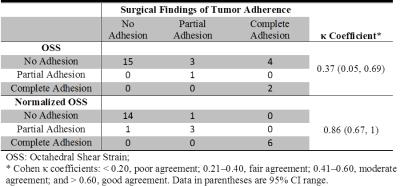
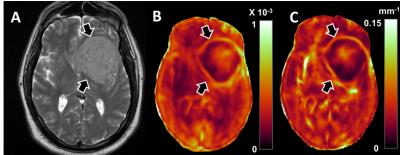
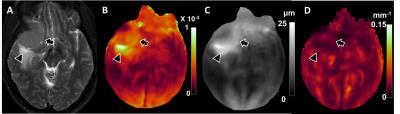
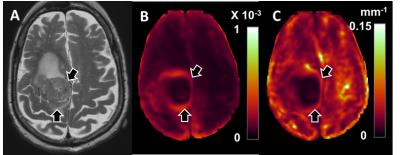
As shown in Tab.2, neurosurgeons categorized tumor as no adhesion in 15 patients, partial in 4 and complete adhesion in 6. OSS characterized 22 tumors as no, 1 as partial, and 2 as complete adhesion, whereas normalized OSS assessed 15 as no, 4 as partial, and 6 as complete adhesion. OSS agreed with the surgical findings in 18(72%) cases (fair agreement with κ=0.37, 95%CI 0.05-0.69), while normalized OSS was concordant with the surgical findings in 23(92%) cases (good agreement with κ=0.86, 95%CI 0.67-1). The correlation between SII predictions (OSS and normalized OSS) and the surgical findings were statistically significant (p=0.02 and p<0.0001 respectively). Fig.1 is an example where both OSS and normalized OSS were concordant with surgical findings. Fig.2 is an example of normalized OSS correlating better with surgery than OSS. A discordant case where neither OSS nor normalized OSS agreed with surgical findings is shown in Fig.3.Discussion
SII provides a dynamic measure of tumor adherence based on characterizing the mobility between the tumor and adjacent brain under applied shear force. The existence of a slip interface can be reflected by a discontinuity in wave displacement across the tumor-brain boundary, which is detected as large OSS. All 15 tumors without adhesion were predicted correctly by OSS, however in patients with partial and complete adhesion, 7 of 10 tumors were misinterpreted as no adhesion. Of these 7 discordant cases, all had mild to severe peritumoral edema, and exhibited large displacement amplitude near the tumor-edema interface (Fig.2c), which could be explained by decreased stiffness of brain parenchyma from increased tissue fluid content7. Since shear strain is proportional to the displacement amplitude, an artificial slip interface can result on an OSS map due to the large wave amplitude within the edema (Fig.2b). Normalizing OSS to the wave amplitude partially removed this effect of amplitude variation (Fig.2d). However, normalized OSS failed in two cases; one where the tumor was very soft, and another where the tumor was very stiff (Fig.3). These discrepancies imply that the inherent stiffness contrast of the tumor may also affect the SII results. Future work will focus on understanding how these non-slip shear factors affect the behavior of SII results, and developing a more generalized normalization algorithm.Conclusion
SII preoperatively evaluates the degree of meningioma-brain adhesion noninvasively, possibly allowing for improved prediction of surgical risk and tumor resectability. Normalized OSS provides a more accurate prediction of meningioma-brain adhesion in the setting of peritumoral edema compared to OSS.Acknowledgements
This work was supported in part by grants from the National Institute of Health RO1 EB001981 and an Office of Naval Research Contract N00173-15-P-0618.References
1. Yin Z, Glaser KJ, Manduca A, Van Gompel JJ, Link JM, Hughes JD, Romano A, Ehman RL, Huston J. Slip Interface Imaging Predicts Tumor-Brain Adhesion in Vestibular Schwannomas. Radiology. 2015; 277: 507-517.
2. Mariappan YK, Glaser KJ, Manduca A, Ehman RL. Cyclic motion encoding for enhanced MR visualization of slip interfaces. Journal of Magnetic Resonance Imaging. 2009;30(4):855-63.
3. Murphy MC, Huston J, 3rd, Glaser KJ, et al. Preoperative assessment of meningioma stiffness using magnetic resonance elastography. J Neurosurg. 2013;118(3):643-8.
4. McGarry MD, Van Houten EE, Perrinez PR, Pattison AJ, Weaver JB, Paulsen KD. An octahedral shear strain-based measure of SNR for 3D MR elastography. Phys Med Biol. 2011;56(13):N153-64.
5. Bioucas-Dias JM, Valadao G. Phase Unwrapping via Graph Cuts. IEEE Transactions on Image Processing. 2007; 16(3): 698-709.
6. Kolmogorov V1, Zabih R. What energy functions can be minimized via graph cuts? IEEE Trans Pattern Anal Mach Intell. 2004;26(2):147-59.
7. Xu ZS, Lee RJ, Chu SS, et al. Evidence of Changes in Brain Tissue Stiffness After Ischemic Stroke Derived From Ultrasound-Based Elastography. Journal of Ultrasound in Medicine. 2013;32(3):485-94.
Figures