0683
Extreme ASL: Challenges and Solutions to Improve Perfusion Imaging in Patients with Markedly Prolonged Arterial Transit Delays1Radiology, Stanford University, Stanford, CA, United States, 2GE Healthcare, Calgary, Canada, 3GE Healthcare, Menlo Park, CA, United States
Synopsis
It is known that if labeling parameters are not properly adjusted in the presence of prolonged arterial transit delays (ATDs), perfusion may be underestimated using arterial spin labeling (ASL), yielding false negatives and possibly unnecessary interventions. In this study we evaluate the cases where the prolonged ATDs due to cerebrovascular disease posed challenges to perfusion quantification using ASL. Some possible solutions, which we term ‘extreme ASL’, were explored and discussed.
Introduction
Accounting for arterial transit delay (ATD) effects in arterial spin labeling (ASL) is necessary to accurately measure cerebral blood flow (CBF) 1. Underestimation of CBF occurs when the post-labeling delay (PLD) is insufficient for a given ATD, which can be substantially increased in many cerebrovascular diseases. The most common solution when long ATDs are suspected is to use a longer PLD; however other solutions exist. Multi-delay ASL has the potential to map the ATD and model its effects on CBF 2. Velocity-selective ASL (VSASL) is intrinsically insensitive to ATD 3 and has shown potential in pediatric Moyamoya patients 4. In this study, we investigate the cases where the prolonged ATDs due to cerebrovascular disease posed challenges to perfusion quantification using pseudo-continuous ASL (pcASL) 5, a recommended ASL method 6 with high SNR.Methods
A total of five patients (4 F, 42±7 yrs.) with cerebrovascular diseases (patient 1 with carotid stenosis, patients 2-5 with Moyamoya disease) were studied using a combination of the following ASL variants (all based on a 3D FSE stack-of-spiral acquisition at 3.0T):
1) Standard (STD) single-delay: TR/TE = 4852/10.7 ms, label duration (LD)/PLD = 1450/2025 ms, 8-shot, voxel size = 3.6*3.6*4 mm, averages = 3, scan time = 4:42.
2) Sequential multi-delay (mTI): TR/TE = 6489/10.7 ms, LD = 2000 ms, 5 equally spaced PLDs 700-3000 ms, 4-shot, voxel size = 5.5*5.5*4 mm, averages = 1, scan time = 4:46.
3) Single-delay ASL with long LD and long PLD (LLLD): TR/TE = 8489/10.7 ms, LD/PLD = 3000/4000 ms, 4-shot, voxel size = 5.5*5.5*4 mm, averages = 4, scan time = 5:06.
4) Velocity-selective (VSASL): TR/TE = 4160/10.7 ms, LD/label-image delay = 1590/1600 ms, 4-shot, voxel size = 5.5*5.5*4 mm, averages = 4, scan time = 2:24.
3D time-of-flight angiograms (MRA) and high resolution 3D T1-weighted images were acquired in all subjects. Supratentorial gray matter (GM) masks, divided into left and right ROIs, were created using the T1-weighted images. The CBF and ATD maps from ASL measurements were co-registered to anatomical images and analyzed within the supratentorial GM ROIs.
Results
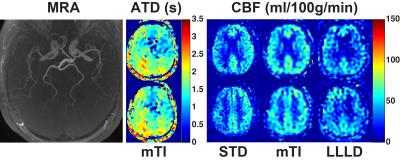
Representative MRA, ATD, and CBF maps in patients 1-5 are shown in Figures 1-3. Figure 1 demonstrated a case with relatively mild ATD artifacts, with some intravascular ASL signal. Multi-delay measurement was able to measure and correct such artifacts, yielding a more balanced perfusion map. In this case, LLLD did not benefit from using a longer PLD; on the contrary, unnecessarily long PLD resulted in less SNR and inferior image quality.
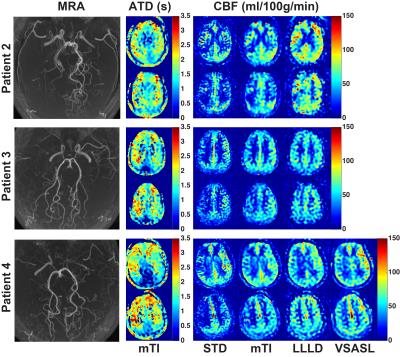
In patients 2-4, ATD artifacts were more severe, with regions of apparent perfusion deficits shown in STD measurement that were not fully recovered by multi-delay measurement. In these cases, LLLD was able to recover almost all the apparent perfusion deficits measured with STD, likely representing the true perfusion status of the brain tissue. In patient 4, VSASL produced CBF maps free of apparent perfusion deficits, showing improved SNR with less than half of the scan time (2:24 vs. 5:06), compared to LLLD.
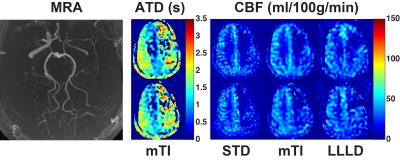
Shown in Figure 3, patient 5 had relatively low flow. The resulting overall low SNR posed a big challenge for all three tested PCASL sequences. Compared to the CBF maps measured with STD sequence, the multi-delay and LLLD methods showed increasingly improved estimates in the anterior and posterior regions on the affected side.
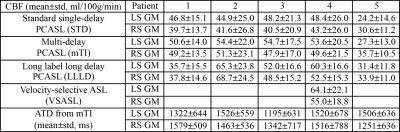
The averaged CBF and TD estimates in the left and right supratentorial GM ROIs are reported in Table 1.
Discussion
Prolonged ATD due to cerebrovascular diseases poses challenges in accurately measuring the brain perfusion with a single-delay pcASL sequence with standard labeling parameters. Multi-delay pcASL can measure the ATD information and improve CBF quantification, but is not always able to recover all the apparent perfusion deficits. Increasing the PLD range and the number of samples at long PLDs in multi-delay pcASL should improve its performance. Single-delay pcASL with LLLD aims at improving SNR of ASL signal while compensating for the prolonged ATDs. Overall, this strategy performed very well, but one should also be aware that if ATD’s are not prolonged, the approach suffers from undesired SNR loss. VSASL showed good promise and SNR advantage in accounting for ATD effects, compared to LLLD pcASL. However, the current implementation still shows some intravascular signals and/or cerebrospinal fluid contamination. With one or more of the above options in labeling methods, ASL may be able to solve the challenges from prolonged ATDs in patients with cerebrovascular disease.Acknowledgements
NIH R01NS066506, R01NS047607, NCRR 5P41RR09784. GE Healthcare.References
1. Alsop, D. C. and J. A. Detre (1996). "Reduced transit-time sensitivity in noninvasive magnetic resonance imaging of human cerebral blood flow." Journal of Cerebral Blood Flow and Metabolism 16(6): 1236-1249.
2. Günther, M., et al., (2001). "Arterial spin labeling in combination with a look-locker sampling strategy: inflow turbo-sampling EPI-FAIR (ITS-FAIR)." Magnetic Resonance in Medicine 46(5): 974-984.
3. Wong, E. C., et al. (2006). "Velocity-selective arterial spin labeling." Magnetic Resonance in Medicine 55(6): 1334-1341.
4. Bolar, D., et al. (2015). Comparison of CBF measured with velocity selective ASL and pulsed ASL in pediatric patients with prolonged arterial transit times due to Moymoya Disease. Proc ISMRM 2015; 778.
5. Dai, W. Y., et al. (2008). "Continuous Flow-Driven Inversion for Arterial Spin Labeling Using Pulsed Radio Frequency and Gradient Fields." Magnetic Resonance in Medicine 60(6): 1488-1497.
6. Alsop, D. C., et al. (2015). "Recommended implementation of arterial spin-labeled perfusion MRI for clinical applications: A consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia." Magnetic Resonance in Medicine 73(1): 102-116.
Figures