0674
Discrimination of Malignant versus Benign Mediastinal Lymph Nodes Using Diffusion MRI with An IVIM Analysis1Radiology, Peking University Cancer Hospital and Institute, Beijing, People's Republic of China, 2Center for MR Research, University of Illinois at Chicago, Chicago, IL, United States, 3Thoracic Surgery, Peking University Cancer Hospital and Institute, Beijing, People's Republic of China, 4Bioengineering, University of Illinois at Chicago, Chicago, IL, United States, 5Radiology and Bioengineering, University of Illinois at Chicago, Chicago, IL, United States, 6Radiology, Neurosurgery, and Bioengineering, University of Illinois at Chicago, Chicago, IL, United States
Synopsis
Noninvasive discrimination of mediastinal lymph nodes (MLN) is crucial for management of cancer patients such as those with non-small cell lung carcinoma. This study aims at investigating the value of IVIM diffusion parameters (D, D*, and f) as well as ADC for discrimination of malignant and benign MLN. A total of 91 MLN from 35 patients with histopathologic proven lesions were studied. D and f of malignant mediastinal lymph nodes were significantly different from those in the benign ones. The combination of f and D produced the highest diagnostic performance as evaluated by a receiver operating characteristic (ROC) analysis.
Background and Purpose
Accurate assessment of the involvement of mediastinal lymph nodes (MLN) of patients with non-small cell lung carcinomas (NSCLC) is essential for properly selecting the patients for surgical resection. With its sensitivity to tissue structural changes, diffusion-weighted imaging (DWI) can be a useful tool in differentiating malignant versus benign MLN. Up to date, DWI studies on MLN almost exclusively rely on ADC, which is prone to confounds introduced by microcirculation of blood, particularly at low b-values. The intra-voxel incoherent motion (IVIM) method can separate microvascular perfusion effects from the intrinsic diffusion process1,2, and can potentially provide additional parameters to improve the differentiating between malignant and benign lesions3. The purpose of this study is to investigate the additional value of the IVIM parameters for discrimination of MLN.Materials and Methods
Thirty five subjects with enlarged lymph nodes in the mediastinum (short axis≥8mm) (23 cases with NSCLC, 12 cases with unknown cause) were scanned on a 1.5T MR scanner. Multi-b-DWI was performed in the transverse plane with an eight-channel body coil. The main parameters for multi-b DWI were: TR/TE=10000/62 msec, FOV≈320~380mm, pixel size≈2.3×2.3 mm2, slice thickness= 5 mm, inter-slice gap = 1.0 mm. Diffusion gradients were applied successively to the three orthogonal axes, producing trace-weighted images with eight b-values of 01, 501, 1001, 2001, 4002, 6002, 8004 and 10004 s/mm2, where the subscript denotes the number of averages. The total scan time for MR-DWI was 6 minutes and 50 seconds.
IVIM analysis was performed using the model proposed by Le Bihan: S = S0 [f e−bD* + (1 − f )e−bD]1. Parameter maps of D, D* and f were generated by fitting the IVIM model to the multi-b diffusion images on a pixel-by-pixel basis using a Levenberg-Marquardt nonlinear fitting algorithm. In addition, ADC map was also produced using software provided by the scanner manufacturer. ROIs were manually drawn on the maximum cross-sectional area in the ADC map4.
Pathologic confirmation of the MLN was obtained in 34 cases and only one case of sarcoidosis was confirmed with the radiologic follow-up study. A total of ninety-one nodes from the 35 patients were analyzed, including 49 malignant and 42 benign nodes based on pathologic or radiologic confirmations.
The IVIM parameter D, D* and f, as well as ADC, were obtained and compared between benign and malignant groups. Receiver operating characteristic (ROC) analysis was performed to evaluate the diagnostic performance.
Results
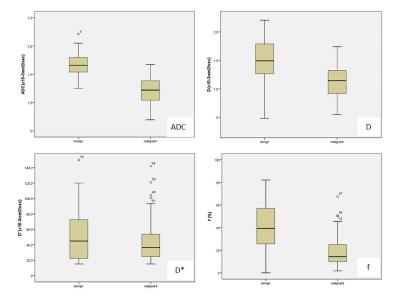
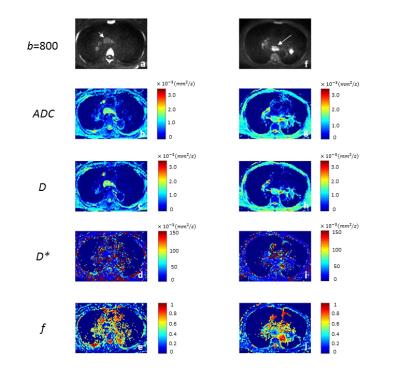
Mean D [1.12±0.28×10-3mm2/sec vs. 1.48±0.40×10-3mm2/sec] and ADC [1.21±0.23×10-3mm2/sec vs. 1.68±0.21×10-3mm2/sec] of malignant MLN were both significantly lower than those in the benign (p<0.001). While D* showed no significant difference (p=0.281), the mean f of the benign MLN (f=41.26±20.12%) was larger than that of the malignant (f=18.78±13.75%) with p<0.001[Figures 1, 2].
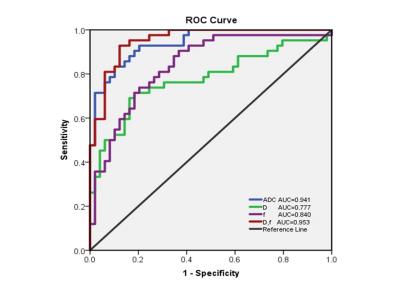
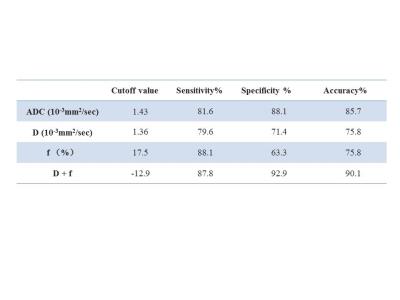
In the ROC analysis (Figure 3), although ADC produced a larger area under the curve (AUC=0.941) and diagnostic accuracy (85.7%; Table 1) than D or f, the combination of D and f provided superior performance in diagnostic accuracy (90.1%) in differentiating MLN malignancy. The optimal cutoff values, sensitivity, specificity, and diagnostic accuracy are summarized in Table 1.
Discussion and Conclusion
Our results were consistent with a previous study on discrimination of lung cancer from focal inflammatory lesions5. To the best of our knowledge, the present study represents the first demonstration that the combination of IVIM parameters can further improve differentiation between benign and malignant MLN as compared to ADC. This improvement is likely related to the combined importance of both cellular and vascular changes during malignancy processes. The moderate, but important, improvement afforded by the IVIM model is expected to help imaging-based non-invasive evaluations of MLN involvement in patients with cancer, such as NSCLC, to determine the best treatment strategies.Acknowledgements
We thank Jun Zhao, Jin-Feng Chen, Jian Fang, and Yu Sun from Peking University Cancer Hospital and Institute for providing support for this study.References
1. Le Bihan D, Breton E, Lallemand D, Aubin ML, Vignaud J, Laval-Jeantet M. Separation of diffusion and perfusion in intravoxel incoherent motion MR imaging. Radiology.1988;168:497–505.
2. Le Bihan D. Intravoxel incoherent motion perfusion MR imaging: a wake-up call. Radiology 2008; 249: 748–752.
3. Iima M, Le Bihan D. Clinical Intravoxel Incoherent Motion and Diffusion MR Imaging: Past, Present, and Future. Radiology. 2016; 278(1):13-32.
4. Joo I, Lee JM, Han JK, Choi BI. Intravoxel incoherent motion diffusion-weighted MR imaging for monitoring the therapeutic efficacy of the vascular disrupting agent CKD-516 in rabbit VX2 liver tumors. Radiology. 2014;272(2):417-26.
5. Deng Y, Li XC, Lei YX, Liang CH, Liu ZY. Use of diffusion-weighted magnetic resonance imaging to distinguish between lung cancer and focal inflammatory lesions: a comparison of intravoxel incoherent motion derived parameters and apparent diffusion coefficient. Acta Radiol. 2015;13. pii: 0284185115586091 PMID: 25972370 DOI: 10.1177/0284185115586091
Figures