0664
Detection and measurement of neuroendocrine tumors liver metastases using Gd-EOB-DTPA enhanced MRI: comparison between multiple arterial phases, hepatobiliary phase, and DWI1Department of Radiology, Peking Union Medical College Hospital, Beijing, People's Republic of China, 2Siemens Ltd, Shanghai, People's Republic of China
Synopsis
The detection and evaluation of liver metastasis (LM) is important in initial staging and follow-up examinations of neuroendocrine tumors patients. Our aim is to compare different sequences including multiple arterial phases (MA), hepatobiliary phase (HA), diffusing-weighted imaging (DWI), and T2WI in Gd-EOB-DTPA-enhanced MRI, to find which sequence is better for detecting LM and which is better for size measurement. MA using CDT-VIBE were superior for the detection of small lesions. HBP imaging shows better repeatability in size measuring and may be a better choice for lesion size measurement during follow-up.
Introduction and Purpose
Neuroendocrine tumors (NETs) showed an increasing incidence in the past years and many patients present with liver metastases (LM)1. The evaluation of LM is important in initial staging and follow-up examinations. However, it remains challenging on one hand to detect all the LM and on the other hand to accurately measure the lesion during follow-up. Multi-arterial-CDT-VIBE allows the acquisition of multiple arterial phases in 1 breath-hold and has the potential to detect more lesions2. Gd-EOB-DTPA is a liver specific contrast agent and has been proved to have advantages in detecting small lesions3,4. The aim of this study is to compare the value of different MR sequences, including multiple arterial phases (MA), hepatobiliary phase (HBP), DWI, and T2WI in evaluating LM in NETs patients.Methods
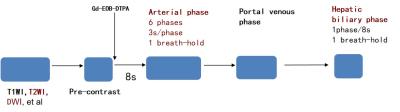
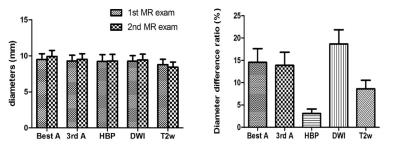
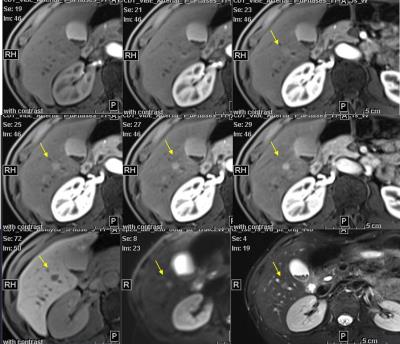
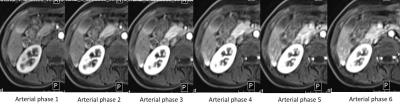
All patients gave written informed consent for this institutional review board-approved study. Between December 2014 and August 2016, 18 NETs patients with liver metastases were examined. The diagnosis of NETs was confirmed histopathologically. Patients were imaged at 3T scanner (Siemens MAGNETOM Skyra) using a 32-channel phased-array body-and-spine coil. MR protocol included T1WI, T2WI, DWI and post-contrast sequences. Gd-EOB-DTPA was injected at a dose of 0.1ml/kg with a flow rate of 2ml/s and flushed with 30ml saline. MA using CDT-VIBE (spatial resolution 1.3×1.3×3mm, time resolution 3.1s, 6 phases, 1 breath-hold) started 8s after the beginning of the contrast agent, followed by portal venous (20s after the completion of arterial phase) and hepatobiliary phase (20min after contrast injection). Numbers of LM detected in different sequences [six arterial phases, best arterial phase (BA), 3rd arterial phase (3A), HBP, DWI, T2WI] were calculated. A liver lesion was considered LM if it was enhanced in arterial phase, hyperintense on T2WI and/or DWI and proved to be LM in the follow up MR exam. In quantitative analysis, contrast ratio between LM and normal liver parenchyma in BA, 3A, HBP, DWI, and T2WI were calculated and compared using paired T test. In qualitative analysis, the overall image quality, artifact, and the delineation of lesion were determined on a 5 grade scale (1 = poor to 5 = excellent) and compared with Mann–Whitney rank sum test. For analyzing the repeatability of lesion size measurement, 6 of the 18 patients who were clinical proved stable were enrolled. The longest diameter of the same lesion in BA, 3A, HBP, DWI, and T2WI was measured on two MR exams (less than 3 months interval) respectively. The diameter difference ratio (|diameter 2- diameter 1|/diameter 1) was compared with paired T test. The diameter of the lesions measured in 6 arterial phases, HBP, DWI and T2WI were also compared with paired T test.Results
In total, 341 liver metastases in 18 patients were detected. All 341 lesions were detected by MA, 327 (96%) by BA, 283 (83%) by 3A, 321 (94%) by HBP, 307 (90%) by DWI, and 181 (53%) by T2WI. The contrast ratio between LM and liver tissue significantly higher in DWI (2.2) than BA (1.6), 3A (1.6), HBP (1.6) and T2WI (1.9) (P<0.05). The lesion delineation in HBP was significantly sharper than BA, 3A and DWI (P<0.05). The overall image quality of HBP, T2WI and DWI is significantly better than 3A (P<0.05). The diameters measured in arterial phase 1 were significantly smaller than arterial phase 2-6, and in HBP significantly smaller than BA and 3A (P<0.05). The diameter difference ratio was significantly smaller in HBP than all other sequences (P<0.05).Discussion
MA were found to be of value in detecting metastases compared to single arterial phase, HBP and DWI. Some small lesions may only show enhancement in 1 or 2 phases and thus can be detected in MA but missed in single arterial phase. HBP has challenge in detecting small lesions near the intrahepatic vasculature since they both present as hypointense small dot. Most lesions present brighter in DWI and may be found more easily, but some small lesions still remain undetectable, and lesions near the edge of liver may be confused with artifact.
HBP is a better choice for lesion size measurement in comparison of arterial phases. In different arterial phases, the enhancement extent of the lesion may vary, and the adjacent liver parenchyma may also show enhancement, influencing the size measurement. In the contrast, lesions in HBP are with sharper delineation and not affected by their enhancement pattern.
Conclusion
MA were superior for the detection of small lesions than single arterial phase, HBP and DWI. HBP shows sharper lesions delineation and better repeatability in size measuring, thus is a better choice for lesion size measurement during follow-up.Acknowledgements
No acknowledgement found.References
1. Frilling A, Sotiropoulos GC, Li J, et al. Multimodal management of neuroendocrine liver metastases[J]. HPB : the official journal of the International Hepato Pancreato Biliary Association, 2010,12(6):361-379.
2. Jinrong Q, Shuai H, Hongkai Z, et al. MBI improved Detection of Recurrent Hepatocellular Carcinomas in Arterial Phase With CAIPIRINHA-Dixon-TWIST-Volumetric Interpolated Breath-Hold Examination[J]. Investigative Radiology, 2016, 51(10):602-608.
3. Shimada K, Isoda H, Hirokawa Y, et al. Comparison of gadolinium-EOB-DTPA-enhanced and diffusion-weighted liver MRI for detection of small hepatic metastases[J]. European radiology, 2010,20(11):2690-2698.
4. Tsurusaki M, Sofue K, Murakami T. Current evidence for the diagnostic value of gadoxetic acid-enhanced magnetic resonance imaging for liver metastasis[J]. Hepatology research : the official journal of the Japan Society of Hepatology, 2016,46(9):853-861.
Figures