0663
Dynamic Contrast Enhanced MR Imaging of Hepatopancreatobiliary lesions in Combined use of Parallel Imaging and Compressed Sensing1Radiology, Seirei Hamamatsu General Hospital, Hamamatsu, Japan, 2Global MR Applications and Workflow, GE Healthcare Japan, Hino, Japan, 3Global MR Applications and Workflow, GE Healthcare, Madison, WI, United States, 4Global MR Applications and Workflow, GE Healthcare, Waukesha, WI, United States, 5Radiology, Hamamatsu University School of Medicine, Hamamatsu, Japan
Synopsis
The feasibility of dynamic Gd-contrast study using turbo LAVA with ARC and CS for evaluation of pancreatobiliary lesions was evaluated. Acceptable image quality and good temporal resolutions with selective recognition of vasculatures, and lesion detections in the liver and pancreas could be made. With this technique, dynamic contrast imaging with high temporal and spatial resolutions can cover the wide area. It takes acceptable time for imaging reconstruction with ARC and CS at clinical 3T MR unit.
Introduction
Breath-hold (BH) dynamic contrast MR study has provided information of characterization of abdominal lesions. To obtain higher temporal and spatial resolution images of the abdomen, faster imaging technique has been desired. Parallel imaging is one of the methods to facilitate faster imaging, but, high acceleration in parallel imaging may induce noise amplification and aliasing artifacts, and its signal intensity (SI) and image quality should be influenced by utilized coil geometry. Combined use of parallel imaging, Autocalibrating Reconstruction for Cartesian imaging (ARC, GEHC) and compressed sensing (CS)1 may allow split acceleration between two fast imaging technique and will give better image quality than ARC alone. The purpose was to evaluate feasibility of dynamic contrast study using 3D imaging technique based on turbo liver acquisition with volume acceleration (LAVA, GEHC) with nonspecific Gd-chelate for evaluations of hepatopancreatobiliary regions using ARC and CS.Materials and Methods
The current study was approved by Institutional Review Board and informed consent was obtained.
Population: Thirty-one patients (15men, 16 women, mean 61years old) who underwent Gd contrast enhanced MR imaging for evaluation of hepatopancreatobiliary lesions. Pathologies were as follows; pancreatic cystic lesions 17cases, Pancreatic cancer 1, Acute pancreatitis 1; Hemangioma 7, Hepatic Cysts 13, A P Shunt 5, Gall Bladder: Cholecystitis GB stone 5, Adenomyomatosis 1, Cholangitis 1, Normal 4, status post Cholecystectomy 2. Pathologies were overlapped in cases.
MR imaging: MR imaging was performed on 3T system (Discovery 750, GEHC) using 32 channel phased-array multicoil. BH dynamic contrast imaging covering liver and pancreas in transverse plane was performed using turbo LAVA with ARC and CS, spec IR. Image reconstruction for ARC and CS was performed by applying CS iterative reconstruction followed by ARC data driven reconstruction1. The following parameters were used: ARC factor 2x1.8, CS factor 1.4, TR 4ms, Matrix 288x224, FOV350mm, slice thickness 4mm/-2mm, one phase 4-5seconds. Five phases of images were obtained during one BH after injection of nonspecific Gd-chelate (ProHance or Magnevist, 0.1mmol/kg, injection rate 3mL/sec). Initial imaging started five seconds after contrast arrival at the level of diaphragm determined by Smart prep. 60 and 90sec after triggering, dual phase imaging for portal and single for equilibrium phase was obtained, respectively. It took five minutes per phase for image reconstruction.
Evaluations: 1) Image quality and artifacts such as blurring related to CS were evaluated using five-point scale (1 non-diagnostic or sever artifacts to 5 excellent quality or no blurring). 2) Selective recognition of enhanced vasculature and pancreas was evaluated, respectively. “A” indicates that hepatic arteries were solely enhanced. “A>P” indicates that hepatic arteries were more enhanced than branches of portal artery in liver. "A<P" indicates that portal vein was less enhanced than hepatic arteries. "A=P" indicates equal enhancement of both vasculatures. “V=” indicates hepatic vein and hepatic parenchyma were equally enhanced. “V+” indicates that hepatic veins were more enhanced than hepatic parenchyma. “Panc” indicated the peak enhancement of pancreatic parenchyma. 3) Subjective Lesion recognitions: Existence of solid or cystic lesions was evaluated. Subjective criteria for recognition of lesions: Liver lesion: Cystic, without enhancement compared with surrounding hepatic parenchyma; Solid, with massive or nodular enhancement; Pancreas; Cystic, Low SI without massive enhancement; Solid, existence of enhanced area in the lesion.
Results
1) In 2nd and later phases, image quality was good and blurring artifacts were less recognized (Fig 1). 2) Precontrast and 1st phase images might have overall lower SI (Fig 2-3). The hepatic arteries were selectively enhanced or dominantly enhanced on 1st to 2nd phase images, and vasculatures were well identified. Peripheral nodular enhancement was noted in hemangioma (Fig 2), which was recognized as solid lesions. 3) Subjective Lesion recognitions: Pancreas; Cystic lesions including IPMN, 17/17cases, Pancreatic cancer 1/1; Liver, Hepatic solid lesions Hemangioma 7/7, Hepatic Cysts; 13/13. All solid and cystic lesions in the liver, pancreatic cystic and solid lesions were correctly identified. Selective enhancement of hepatic vasculatures and pancreatic parenchyma (Table): the hepatic artery was selectively enhanced in 1st phase of 22 cases (Fig 2, 3) and 2nd phase of 8 cases, respectively.
Discussion and Conclusions
Dynamic contrast MR imaging with high
temporal resolutions could be successfully obtained in liver and pancreas. Feasibility
was demonstrated.
The images selectively visualized vasculatures,
cystic and solid lesions in the liver and pancreas. Currently, sequential independent
data are used for image reconstruction without contamination.
Start of imaging can be determined with monitoring
of contrast arrival. Thus, data were efficiently obtained.
Conclusion: Using ARC and CS, BH dynamic contrast MR study for hepatopancreatobiliary lesions can be performed with acceptable image quality and lesion and selective vascular recognitions at clinical 3T system.
Acknowledgements
References
1) King K, Xu D, Brau AC, et al. A new combination of compressed sensing and data driven parallel imaging. Proceedings of the Annual Meeting of ISMRM. Stockholm, 2010. (p4881)
Figures
Fig 1 Image Quality and Artifacts in Dynamic contrast imaging
In the 2nd and later phases, scores for image quality and blurring artifacts are high. The contrast enhancement in field of view improves overall image quality.
Table Selective enhancement of the Hepatic vasculatures and Pancreas
Numbers indicates number of cases, where the following features were observed.
A:Artery,
P: Portal vein, V: Hepatic vein, Panc; Pancreas.
Fig 2 Hemangiomas 50's women
In the 1st phase, the hepatic artery is solely enhanced and recognized well. Peripheral nodular enhancement is noted in the lesion, which increases with time, indicating solid lesion, hemangioma. In the 2nd phase, the portal vein is enhanced.
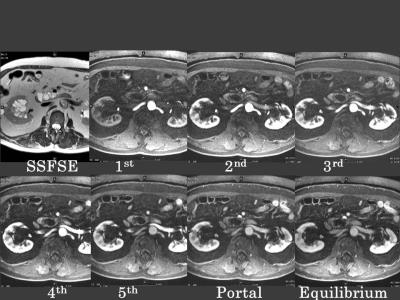
Fig 3a IPMN 70's Man
Images at the level of the pancreas. In the 2nd phase, the pancreatic parenchyma is getting enhanced although there are no enhancements in the lesions of the pancreatic head. The peak enhancement of the pancreas is noted in the 2nd phase of the image.
Fig3b IPMN 70's Man
Images at the level of the liver. The hepatic artery is well recognized in the 1st phase, and the portal vein is getting enhanced in the 3rd phase. In the 4th and 5th phases, the hepatic artery in the posterior segment is not recognized due to the strong enhancement of the portal vein.