0650
Ability of MAVRIC MRI to Predict Component Loosening in Total Hip ArthroplastyAlissa Jo Burge1, Gabrielle P Konin1, Jennifer Berkowitz1, Matthew Koff1, Douglas Padgett2, and Hollis Potter3
1Radiology and Imaging, Hospital for Special Surgery, New York, NY, United States, 2Adult Reconstruction and Joint Replacement, Hospital for Special Surgery, New York, NY, United States, 3Hospital for Special Surgery, New York, NY, United States
Synopsis
Improved metal reduction techniques for conventional MRI pulse sequences and the addition of MAVRIC (multiacquisition variable resonance image combination) have been established as useful in assessing component osteolysis and synovial reactions. The purpose of this retrospective study was to determine the utility of MRI in assessing loosening of total hip arthroplasty in a cohort of patients using surgical confirmation of loosening as the gold standard. Our results show that loosening can be predicted with high sensitivity and specificity; however, intraoperative variability in assessing loosening and the overall low frequency of implant loosening are limiting factors.
Purpose
MRI is a valuable tool with which to assess total hip arthroplasty (THA) (1). Metal artifact reduction using the MAVRIC (multiacquisition variable resonance image combination) sequence better evaluates the bone implant interface and the osseous integration of hip arthroplasty components. A preliminary retrospective study was performed to determine the accuracy and inter-examiner reproducibility of assessing femoral and acetabular component loosening from MR images, as validated at time of revision THA surgery. Our hypothesis was that the superior soft tissue contrast of MRI would provide an accurate assessment of the fibrous interface encountered at the implant-bone interface in the setting of aseptic loosening.Methods
Following IRB approval with informed consent, a keyword search of the HSS PACS for “MAVRIC” and “hip” with date parameters of January 1st, 2012 through August 1st, 2015 was conducted and the search results were then cross-referenced with the biomechanics implant registry database to identify patients who underwent THA explantation. A total of 58 hips in 57 patients (24M/33F) had preoperative MR imaging available for evaluation. Mean time (±SD) between imaging and revision surgery was 74±65 days. Operative notes were reviewed in order to determine the presence of loosening at the time of surgery. Images were analyzed by zones for relative integration/osseous resorption about the components. The Gruen zones were utilized for evaluation of the femoral component and the acetabular component was divided into anterior/middle/posterior/superior zones. The presence of periprosthetic bone marrow edema was assessed, and each periprosthetic zone was assigned a score of 0, 1, or 2, corresponding to “integrated,” “fibrous membrane formation,” or “osteolysis”, respectively. Finally, each radiologist concluded whether the acetabular or femoral component was overtly loose.Results
Near perfect agreement was found for imaging assessment of loosening in a majority of regions about the acetabular component: Anterior κ=0.82 (95%CI: 0.69 to 0.95), Posterior κ=0.84 (95%CI: 0.71 to 0.96), Superior κ=0.81 (95%CI: 0.68 to 0.93). The Middle region had moderate agreement (κ=0.63; 95%CI: 0.47 to 0.80). Overall reader agreement was excellent (κ=0.87, 95%CI: 0.69 to 1.0). Along the femoral component, perfect or near perfect agreement was found in a majority (9/14) of Gruen zones. Perfect agreement was found in Gruen zones 3, 4, 5, 10, 11 and 12 (κ=1.0). Substantial agreement was found in Gruen zone 2 (κ=0.74, 95%CI: 0.47 to 1.00), zone 9 (κ=0.66, 95%CI: 0.03 to 1.0), and zone 14 (κ=0.72, 95%CI: 0.56 to 0.88). Overall reader agreement for component loosening was perfect, κ=1. When correlating imaging findings with operative findings, we found excellent specificity for femoral loosening: 1.00 (95%CI: 0.92 to 1.00), and acetabular loosening: 0.96 (95%CI: 0.86 to 0.99), and greater sensitivity for acetabular loosening: 0.64 (95%CI: 0.35 to 0.85), than femoral loosening: 0.17 (95%CI: 0.01 to 0.64). The overall femoral positive predictive value and negative predictive values were excellent: 0.89 (95%CI: 0.57 to 0.98) and 0.94 (95%CI: 0.84 to 0.98), respectively. The overall acetabular positive predictive value and negative predictive values were also excellent: 1.00 (95%CI: 0.05 to 1.00) and 0.91 (95%CI: 0.80 to 0.97), respectively.Conclusion
MRI is capable of detecting loosening of THA components, with high sensitivity and specificity for detecting acetabular component loosening. MRI sensitivity of femoral loosening was limited, but this may be at least partially attributed to the non-uniform means by which loosening is assessed intraoperatively, depending on the degree of surgeon distraction of the components at revision. In addition, the presence of cement in 5/6 of loose femoral components was a confounding factor, given the limited contrast between the metallic stem and the inner sleeve of the cement mantle. Additional limiting factors include a low frequency of implant loosening within this initial group of patients, and the fact that quantification of integration was not performed on the current cohort of retrieved implants, factors which will be addressed going forward in an ongoing prospective evaluation of implant integration.Acknowledgements
No acknowledgement found.References
1. Hayter et al; AJR 2011; 197:405-11Figures
Figure
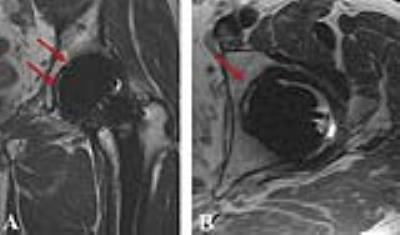
1: Coronal proton density (A) and axial proton density (B) images demonstrate circumferential
fibrous membrane formation along the acetabular component (red arrows), which
was deemed loose both by imaging criteria and intraoperatively.
Figure
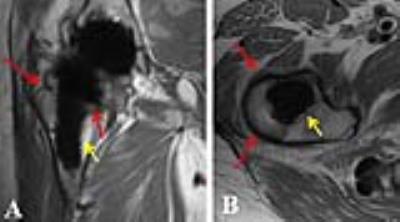
2: Coronal MAVRIC proton density (A) and axial proton density (B) images
demonstrate proximal femoral osteolysis (red arrows) about an arthroplasty
deemed loose intraoperatively; however, as osseous resorption was incomplete on
MRI (yellow arrows), component was not characterized as loose by imaging criteria.