0636
Using transient intrinsic torsional shear wave propagation to measure Left Ventricular Myocardial stiffness with a 2D pencil beam navigator at 0.5ms temporal resolution: Initial results from phantom studies and volunteers1Imaging Sciences & Biomedical Engineering, King's College London, London, United Kingdom, 2Department of Cardiology, Guys and St Thomas' NHS Trust, London, United Kingdom, 3Department of Radiology, Academic Medical Center, Amsterdam, Netherlands, 4Department of Chemical Engineering, Universitat Ramon Llull, Barcelona, Spain
Synopsis
Heart Failure with preserved Ejection Fraction is common, associated with high morbidity and mortality, and is challenging to diagnose. We have developed a novel patient friendly non-invasive technique to quantify myocardial stiffness using transient MR Elastography. Aortic valve closure results in a shear wave propagating through the myocardium. The torsional wave propagation can be visualised using a 2D pencil beam navigator positioned along the myocardium, using four breath holds each 15 seconds. With a temporal resolution of 0.5ms this technique can be used in all patients in sinus rhythm. Increased myocardial stiffness results in increased speed of shear wave propagation.
Background
Heart Failure with preserved Ejection Fraction (HFpEF) is increasingly common and associated with high morbidity and mortality (1). It is hypothesized that HFpEF is characterised by increased myocardial stiffness and our preliminary data using transient MR-Elastography utilizing the aortic valve closure as an intrinsic source for the generation of shear waves, has validated this hypothesis (2). Our previous approach had the drawback that imaging had to be timed minutely to the exact time-point of valve closure and that only one single snap-shot of the propagating wave could be acquired. Thus, only wavelength could be measured and its conversion to shear wave speed and thereby material properties was not evident. To overcome these limitations, we further developed the method to enable the visualization of the torsional wave propagation through the myocardium at temporal resolutions of 0.5ms with 4 consecutive breath-holds.Methods
This study has 3 parts: sequence development, validation of wave speed measurements in phantom models and a volunteer study (n=7).
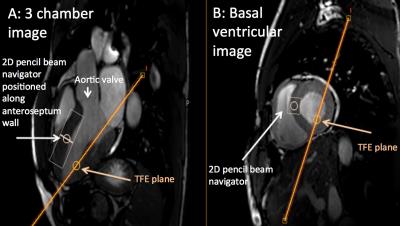
We modified an ECG-gated CINE low-resolution turbo field echo (TFE) sequence. A motion sensitised 2D pencil beam navigator (cRNAV, length 60mm, diameter 25mm) is added before each TFE shot, and the phase data from the navigator are recorded. The total cRNAV shot length (navigator – 25ms; TFE shot – 5ms) is 30ms. The total number of consecutive cRNAV shots covers ~80% of the cardiac cycle, with the rest as a time buffer and allowing for patients with different heart rates to be scanned. Motion sensitisation is possible in all three orthogonal directions (fMEG=160Hz) allowing to uniquely select the torsional wave. Unlike the flexural and compressional wave components, which are biased in their speed by geometry, the torsional wave component propagates unbiased and can hence be used to infer the intrinsic properties of the material. The navigator is positioned (figure 1) along the anteroseptal wall of the myocardium. Temporal resolution of 0.5ms is achieved by increasing the initial delay after the detection of the R wave in each consecutive heartbeat. The phase data is then reordered and the shear wave speed can be calculated by fitting to the space/time waterfall plot. Increased myocardial stiffness will result in increased speed of shear wave propagation.
Results
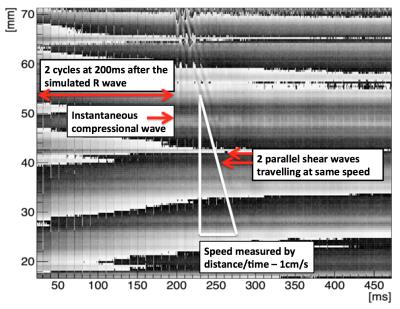
Phantom experiments using known material stiffness demonstrated that the CINE cRNAV sequence measured the correct shear wave speeds at 80Hz with two cycles (figure 2). The fast compressional wave is seen that is almost instantaneous, with two slower shear waves. Both of these had speeds measured at 1m/s, which is identical to the true material stiffness.
3D finite-element simulations confirmed the existence of a torsional wave generated by aortic valve closure propagating at a speed that corresponded to the true shear stiffness of the myocardium used for the simulation.
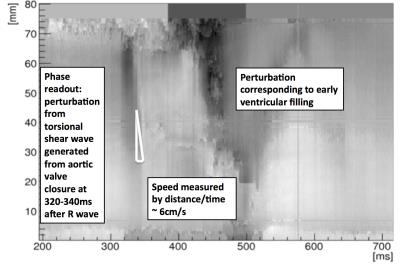
Torsional shear waves were observed in seven healthy volunteers between 300-350ms after the R wave, corresponding to valve closure time. Wave speeds of 5-7m/s were observed resulting in shear modulus estimates of 25-49kPa, (figure 3).
Discussion
This innovative sequence design has allowed us to overcome the challenges we faced previously, and so myocardial shear wave speeds can be calculated with significantly improved temporal resolution. Importantly our phantom and 3D finite element simulations have confirmed the validity of our technique and the unbiased nature of the torsional wave. This is in agreement with the theory for wave propagation in hollow cylinders and opens the gateway to measure cardiac biomechanics non-invasively without the need for external transducers.
The sequence does not rely on prior knowledge of exact valve closure time, which requires additional scans and which can change during the scan as the heart rate increases or decreases. This has resulted in a sequence that is patient friendly, requires no external vibration, is easy tolerated and can be applied to any patient in sinus rhythm.
We plan to use this sequence in patients with confirmed HFpEF that are already undergoing other imaging and pressure volume loop studies. We are also working on using smaller cRNAV diameters and improving temporal resolution further.
Conclusion
We have successfully developed and applied a new patient friendly technique to quantify myocardial stiffness in vivo from torsional shear waves generated by aortic valve closure, not requiring any external transducers. Together with our previous preliminary data in HFpEF patients, this method has significant potential to become an important diagnostic tool for the early detection of pathologically altered myocardial stiffness. Early detection of patients with HFpEF will facilitate better treatment of the condition that will result in improved patient outcome.Acknowledgements
Imaging Sciences & Biomedical Engineering Division Kings CollegeReferences
1 Owan TE, Hodge DO, Herges RM et al. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006; 355:251–9.
2 Webb J, Holub O, Clough R et al. Using intrinsic Cardiac Shear Waves to measure Myocardial Stiffness: Initial results on a Patient Cohort with Heart failure with preserved Ejection Fraction. Proc. Intl. Soc. Mag. Reson. Med. 2016;24:0412.
Figures